Telehealth Reverse Diabetes With Improved Sleep | Free Trial In Texas

If you have Diabetes, get checked for Sleep Apnea! Severe Sleep-Disordered Breathing greatly increases the severity of Diabetes even without Overweight/Obesity.
Relieving sleep apnea immediately improves how you feel and how well you work during the day.
Sign Up
Visit our website: www.herdhealthcare.com, or call us at 713-669-0271 to get started on an action plan for good health.
Duration And Quality Of Sleep: Risk For Diabetes
Sleep duration and risk of type 2 diabetes has been reported in 11 clinical studies. Cases included approximately 500K Caucasian and Asian adults followed for 2.5 to 16 years. A total of 18K cases developed type 2 diabetes during follow-up. The lowest incidence of type 2 diabetes occurred in cases who slept 7-8 hours per day.
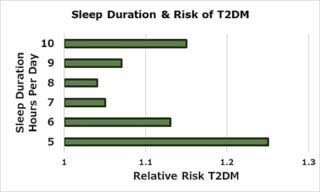 The figure shows that risk of type 2 diabetes increased about 10% for every hour shorter or longer than lowest rate observed at 7-8 hours per day. Laboratory studies using groups with shorter and longer duration showed specific differences.
The figure shows that risk of type 2 diabetes increased about 10% for every hour shorter or longer than lowest rate observed at 7-8 hours per day. Laboratory studies using groups with shorter and longer duration showed specific differences.
Shorter sleep duration was associated with increased neuroendocrine function including sympathetic nervous system activity. As a result, shorter sleep duration caused increased levels of insulin in relation to levels of glucose in blood.
Longer sleep duration was associated with poor physical health, low physical activity and undiagnosed medical illness.
 Quality of sleep has a direct effect on risk of type 2 diabetes. Sleep-disordered breathing has been studied prospectively in 1,453 cases in the U.S. Approximately half had mild to severe sleep-disordered breathing and 6% had severe sleep apnea. During follow-up of 13 years, cases with normal breathing had a 17% risk of developing diabetes. Risk for those who had severe sleep apnea was 35%. This greater risk was independent of both overweight/obesity and maximum waist circumference.
Quality of sleep has a direct effect on risk of type 2 diabetes. Sleep-disordered breathing has been studied prospectively in 1,453 cases in the U.S. Approximately half had mild to severe sleep-disordered breathing and 6% had severe sleep apnea. During follow-up of 13 years, cases with normal breathing had a 17% risk of developing diabetes. Risk for those who had severe sleep apnea was 35%. This greater risk was independent of both overweight/obesity and maximum waist circumference.
Severe Sleep Apnea and Mortality
Sleep studies in Wisconsin have been made in 1520 men and women at 4-year intervals for 18 years.

During that time, 76% of men and women 30 to 60 years of age showed normal breathing patterns. Mildly abnormal breathing patterns were noted in 15%, moderately abnormal patterns in 5% and severe sleep apnea in 4%.
During the next 18 years, mortality rate for cases with normal breathing patterns was 4%. Those with mild or moderate rates of sleep apnea had mortality rates of 7% and those with severe sleep apnea had mortality rates of 19%.
The Mortality Hazard Ratio was 3-fold greater for those with severe sleep apnea compared to those with normal patterns of breathing during sleep. This represents more than 10 years loss of healthy life for those with severe sleep apnea.
Obesity And Obstructive Sleep Apnea
Relation to Body Mass Index in both men and women showed substantially greater occurrence of severe sleep apnea in those with Overweight/Obesity.
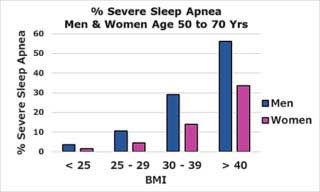 As shown in the figure, men who were Overweight had a 3-fold increase in severe sleep apnea and those who were Obese had a 5-fold increase. Women who were Overweight had a 2-fold increase and those who were Obese had a 5-fold increase.
As shown in the figure, men who were Overweight had a 3-fold increase in severe sleep apnea and those who were Obese had a 5-fold increase. Women who were Overweight had a 2-fold increase and those who were Obese had a 5-fold increase.
Overweight/Obesity brings incredibly great risk for severe sleep apnea and remarkably increased rates of mortality!
Recent trends in occurrence of sleep apnea showed rates of severe sleep apnea for men 50 to 79 years of age have increased from 5.4% in 1990 to 7.0% in 2008. Rates for women have increased from 2.6% to 3.2%.
Increase in Overweight/Obesity and increase in Sleep-Disordered Breathing are parallel epidemics. Although both are connected and increasing, there are independent factors operating.
Type 2 Diabetes and Obstructive Sleep Apnea (OSA)
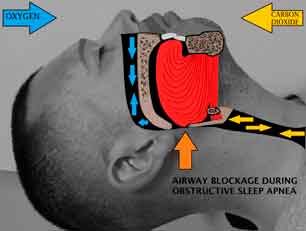
Defining Obstructive Sleep Apnea includes oxygen desaturation criteria. With cutoff criteria of 4%, OSA is reported in 58% of obese diabetic patients.
 With less stringent criteria of 3%, OSA occurs in 77%. Whichever criteria are chosen, it’s likely only 18% of all patients with diabetes and OSA are correctly identified. That would include only 23% of patients with obesity and type 2 diabetes.
With less stringent criteria of 3%, OSA occurs in 77%. Whichever criteria are chosen, it’s likely only 18% of all patients with diabetes and OSA are correctly identified. That would include only 23% of patients with obesity and type 2 diabetes.
Occurrence Of Type 2 Diabetes In OSA ranges from 15 to 30%. Increasing severity of sleep apnea may be a predictor of diabetes. However, we don’t know whether OSA causes diabetes in some patients.
Glucose Control In Untreated Obstructive Sleep Apnea (OSA)
OSA is treatable but frequently goes untreated in patients with type 2 diabetes. Using hemoglobin A1c (HbA1c) as an index of success in controlling diabetes, shows us whether OSA interferes with management of diabetes.
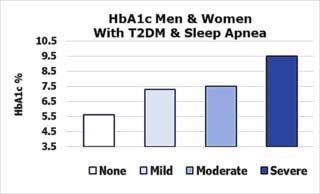 Testing effects of OSA was done in 60 patients with diabetes treated in Chicago. A total of 77% had mild to severe sleep apnea. Measures of age, sex, race, medication, exercise and years of diabetes were balanced between those with and without OSA.
Testing effects of OSA was done in 60 patients with diabetes treated in Chicago. A total of 77% had mild to severe sleep apnea. Measures of age, sex, race, medication, exercise and years of diabetes were balanced between those with and without OSA.
As shown in the figure, the more severe the untreated OSA, the greater the HbA1c. Compared to patients without OSA, those with untreated OSA had substantially higher levels of HbA1c. Those with severe sleep apnea had adjusted HbA1c levels 3.7% higher than those with normal breathing patterns.
Results of this study indicate that effective treatment of OSA could be a safe, nonpharmacologic treatment in management of patients with type 2 diabetes.
Immediate Metabolic Effects of Continuous Positive Airway Pressure (CPAP)
Metabolic effects of OAS occur immediately when CPAP is withdrawn. We know that OAS causes elevations in fat (TGs), fatty acids (FFA) and sugar (glucose) circulating in the blood. OAS also causes elevations in insulin and cortisol, a “fight or flight” steroid hormone secreted by the adrenal glands.
 One effect of cortisol is to cause release of glucose by the liver. Another is to decrease uptake of glucose by skeletal muscle. Both these actions prevent uptake of glucose into liver and skeletal muscle. The result is to increase levels of glucose in the blood for uptake into the brain.
One effect of cortisol is to cause release of glucose by the liver. Another is to decrease uptake of glucose by skeletal muscle. Both these actions prevent uptake of glucose into liver and skeletal muscle. The result is to increase levels of glucose in the blood for uptake into the brain.
The effect of CPAP on metabolic effects of OAS were studied in 31 overweight/obese men and women in Baltimore who had moderate to severe sleep apnea. Type 2 diabetes was present in 7 subjects. All 31 regularly used CPAP and had normal metabolic function during its use.
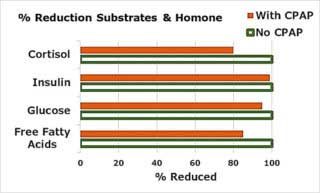 Tests of metabolic function were done on the 3rd night after discontinuing CPAP. Stopping CPAP caused OSA in all subjects. As shown in the figure, stopping CPAP also caused elevations in glucose and FFA circulating in blood as well as increased levels of cortisol and insulin.
Tests of metabolic function were done on the 3rd night after discontinuing CPAP. Stopping CPAP caused OSA in all subjects. As shown in the figure, stopping CPAP also caused elevations in glucose and FFA circulating in blood as well as increased levels of cortisol and insulin.
Glucose levels were markedly elevated in subjects with diabetes. OSA did not increase glucose in those with normal glucose metabolism.
Results of this study demonstrated that CPAP is safe and effective in the treatment of OSA. It provides immediate results to counter the toxic effects of excess calories causing metabolic overload.
Executive Cognitive Dysfunction In Obstructive Sleep Apnea (OSA)
Executive functions of the brain are located primarily in the frontal lobe of the brain. From there, executive cognition controls subconscious cognition that guides physical, mental and emotional function.
Results of OSA on cognitive function have been analyzed in 35 clinical studies. These studies included 551 healthy control subjects and 1,010 subjects with OSA.
 All domains of executive function had medium to very large impairment in OSA. In addition, all executive functions were improved with CPAP treatment.
All domains of executive function had medium to very large impairment in OSA. In addition, all executive functions were improved with CPAP treatment.
Conscious, alert executive cognitive function operates to analyze, plan, organize, schedule and complete goal-oriented tasks. It also includes self-awareness and self-monitoring. Consequently, when executive functions fail, that person is not aware of functional deficits.
Consequently, OAS causes executive cognitive dysfunction without that person realizing there’s a problem with mental function.
Protocol To Improve Duration And Quality Of Sleep
Develop a Sleep Routine For Good Sleep Hygiene.
• rule-out sleep disorders including sleep apnea
• consistent sleep schedule
• reduce noise and light
• cool temperature (70 F, 20 C)
• avoid alcohol, cigarettes, caffeine and heavy meal before retiring
 • pre-sleep routine to relax 60 minutes before retiring
• pre-sleep routine to relax 60 minutes before retiring
• relaxing bath or shower
• comfortable bed, mattress and pillow
• regular exercise (but not before bed)
• restrict evening fluid intake
• sleep diary
 We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com




2 comments
Oralia De Los Santos
April 11, 2019 at 6:29 am
I just left an email address,im a type 2 diabetes. Don’t know how to start explaining myself ive had my Grandparents my Aunt’s my My think God she still alive but shes I’ll, so its so hard for me to really take care of myself cuz im taking care of my Mom like rigjt now im not able to sleep cuz either het pressure to high or suger level so times i don’t check myself.so how does this work i have no money.
Dr. J A Herd MD
April 15, 2019 at 7:54 pm
I would like to help you with your Type 2 Diabetes.
What we do in our program is use telehealth to communicate with you each week
to improve, and maybe reverse Diabetes.
You must have an internet connection to use our server. We will send you a Daily
Health Journal. You will let me know important details about what you do now to
manage your diabetes.
We will set up a Coaching session once a week, at a time that is convenient for
you, to review your records. Together we will map out an action plan to make
gradual improvements.
We offer a free trial for the first 4-6 weeks of our program. During this time you
will find out if Telehealth Coaching is beneficial for you.