COVID-19 Variants
Coronavirus-2 causes serious illness and it’s not going away anytime soon.
So far, about 10% of adults in the US have been sick from COVID-19. Another 5% had infection but no symptoms. Of those with symptoms about 20% have been hospitalized for treatment.
To learn more about programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
COVID-19 And Influenza
Illness with COVID-19 is much more serious than seasonal influenza.
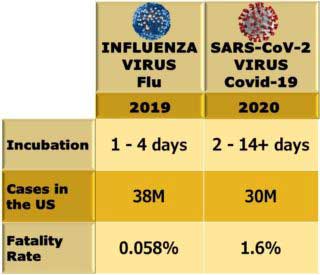 Much greater impact. In 2019, there were about 10% of adults who were sick from influenza and 5% with no symptoms. But only 1% of those with symptoms were hospitalized.
Much greater impact. In 2019, there were about 10% of adults who were sick from influenza and 5% with no symptoms. But only 1% of those with symptoms were hospitalized.
Rates of infection with and without symptoms are about the same. But death rates for those with COVID-19 are more than 20 times higher.
Virus Mutation
Viruses are merely organic structures that can’t move or reproduce. They can’t generate energy. They have no functional capacity until they connect with materials in living cells.
Once connected inside living cells they multiply rapidly. With multiplication, constantly forming new protein, haphazard changes cause mutation. Most new molecules simply disappear. But some have new functional capacity with genes and traits that form new variants.
Virus Variants
Most of these variants are little different than the original forms. But some have traits that allow them to multiply and become dominant. Those that are successful grow and spread through living tissue. They frequently resist immune functions which controlled the original form of the virus.
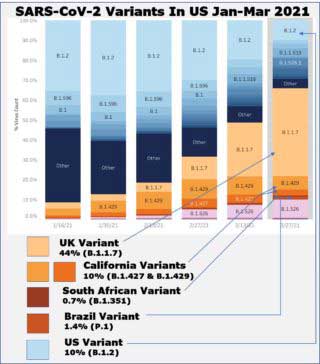
The first variant associated with increased rate of spread appeared in the fall of 2020. Identified in the UK, it has been labelled UK Variant-B.1.1.7. Its most obvious effect is to increase the rate of transmission from person to person. Severity of illness and death rates have not been increased. So far, existing vaccines have provided effective protection from illness and death.
The first variant associated with a decreased immune response was detected in South Africa. It has been labelled South Africa Variant-B.1.351. It changes the shape of proteins attached on cell surfaces increasing its resistance to antibodies of existing vaccines.
Additional variants have been identified in Brazil and the United States. So far, all these variants have been found in most of the United States. Vaccines used in this country to prevent Coronavirus provide protection from all variants discovered so far. However, the continuing spread of viruses and the process of mutation eventually will produce variants that escape immunity from vaccines. Until about 70% the population is vaccinated or recovered from COVID-19, epidemic spread of the virus will continue.
We still don’t know how long immunity lasts after COVID-19 infection or vaccination. Also, we don’t know how frequently variants will appear that require booster injections or new vaccine formulations. It is possible that revaccination will be required every year or two.
This spread of Coronavirus will go on for a while. We have been expecting that vaccines will prevent and medications will cure COVID-19. Then everything would return to normal. But not everybody will get vaccinated, we don’t have any cures for this respiratory virus disease and variants will keep appearing.
We already know that public health measures do not provide complete protection from Coronavirus infection.
We do know that self-protection measures reduce prevalence and severity of Coronavirus infection. Good health habits prevent this respiratory virus disease and reduce its severity.
Innate And Adaptive Immunity
The immune response to COVID-19 infection has two components. It includes immediate cellular action followed by slower action of cells producing antibodies. Both components include hormonal and humoral agents.
The immediate response operates through white blood cells, dendritic cells and macrophages carrying pattern recognizing receptors. Detection of common chemicals, toxins and infectious agents elicits responses to destroy or isolate them. At the same time, the immediate response initiates local inflammation and signals systemic responses. This is the innate immune system. It continuously protects against damaging effects of injury, foreign substances and infectious agents.
The delayed response operates more slowly through white blood cells called B cells and T cells. Antibodies, proteins produced in B cells, are released into blood and attached onto invading cells and foreign substances. T cells directly kill cells that have been infected. Cell debris and foreign material are removed by macrophages.
Risk Factors For COVID-19
The risk factors for severe COVID-19 include comorbidities and physical inactivity. Comorbidities include hypertension, diabetes, obesity, cardiovascular disease and chronic lung disease. Physical inactivity includes complete lack of regular exercise.
Exercise Reduces Risk
General guidelines for physical activity include 150 minutes per week of moderate aerobic, endurance exercise and 2 or 3 sessions of resistance, strength training. Categories of endurance exercise include less than 10 minutes/week, 11 to 149 minutes/week and 150 minutes of exercise spent consistently week after week.
In the Kaiser Permanente Southern California health plan, patients are evaluated at every outpatient visit. About one-third of patients report less than 10 minutes/week and one-third report some exercise. Less than one-third exercise consistently at least 150 minutes/week.
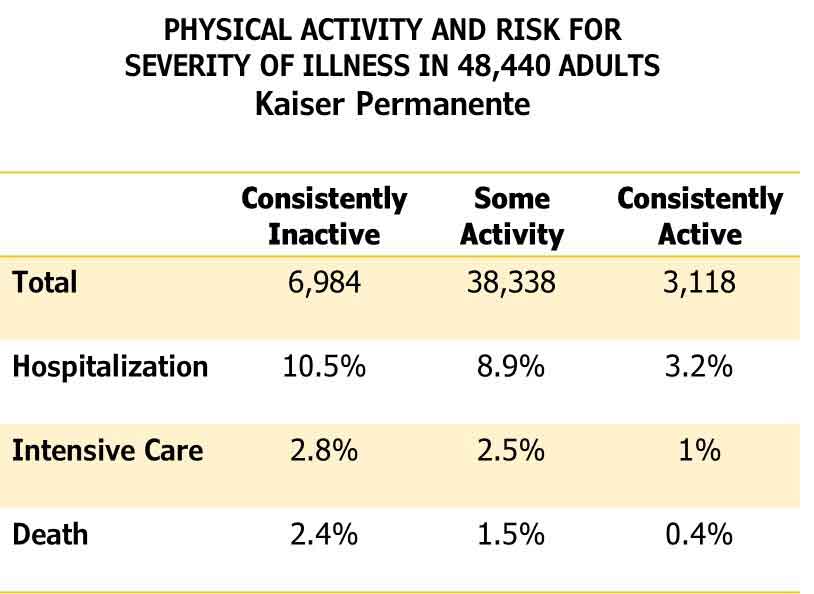 Since January 2020, more than 100,000 patients with a diagnosis of COVID-19 were identified. Approximately 48,000 had at least three reports of exercise since March 2018. Exercise assessments revealed that 14% were inactive, 80% were inconsistently active and 6% consistently exercised at least 150 minutes/week.
Since January 2020, more than 100,000 patients with a diagnosis of COVID-19 were identified. Approximately 48,000 had at least three reports of exercise since March 2018. Exercise assessments revealed that 14% were inactive, 80% were inconsistently active and 6% consistently exercised at least 150 minutes/week.
Hospitalization for treatment of COVID-19 was required for more than 4,000. This was 8.7% of all who had at least 3 assessments of exercise before illness. Among those who had been consistently inactive, 10.5% were hospitalized and eventually discharged, 2.8% were hospitalized and admitted to an Intensive Care Unit. Another 2.4% died.
In comparison, 3.2% of those who had been consistently active were hospitalized and eventually discharged, 1% were hospitalized and admitted to an Intensive Care Unit and another 0.4% died.
More than 15% of those consistently inactive were severely ill or died from COVID-19 compared to less than 5% of those consistently active.
Range of Individual Responses
Severity of illness from COVID-19 infection varies considerably. From complete absence of symptoms to rapid progression of respiratory, cardiac and renal failure.
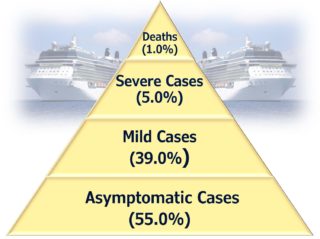 An outbreak of COVID-19 on a cruise ship had 18.5% of all people infected. Of these, 55% were asymptomatic, 39% were mild cases, 5% were severely diseased and 1% died. The majority of people liable to exposure were not infected. Most of those infected were asymptomatic or suffered only mild illness.
An outbreak of COVID-19 on a cruise ship had 18.5% of all people infected. Of these, 55% were asymptomatic, 39% were mild cases, 5% were severely diseased and 1% died. The majority of people liable to exposure were not infected. Most of those infected were asymptomatic or suffered only mild illness.
Genetic risk factors apparently affect risk. Genomic regions associated with coronavirus infection and illness have been identified. Also, large numbers of variable epigenetic features determine the strength of genetic risk.
Epigenetic features vary according to physical fitness, nutrition and psychological factors. All of which determine liability for infection and severity of illness.
Comorbidity Increase In Risk
Comorbidities of obesity, hypertension and diabetes more than double the risk of severe illness from COVID-19. Especially after 75 years of age. Nearly two-thirds of patients hospitalized with COVID-19 suffered from these conditions. There was obesity in 30%, hypertension in 26% and diabetes in 20%. Many had two or even three of these conditions.
Unfortunately, these conditions are common. In the U.S. about three quarters of adults are overweight or obese, about half have hypertension and nearly half have prediabetes or diabetes. All these are preventable.
Overeating And Insulin Resistance
These conditions are particularly affected by overeating. Consuming more than can be used or safely stored.
Within safe limits, between meals and overnight, sugar and fat can be stored in muscles, liver and subcutaneous fat. The amount that can be stored is limited by individual ability to increase fat storage. Some individuals can create enormous numbers of subcutaneous fat cells. Others are severely limited.
Chronic Inflammation
When all available fat cells are full, excess sugar and fat builds up in the blood. Increased levels in blood stimulate the pancreas to produce more and more insulin. Those increased levels of insulin force sugar and fat from blood into cells in skeletal muscle, liver, fat, pancreas, nerves and brain. The result is damage to cells from high levels of insulin, sugar and fat. Some damage is caused by excess fat and some is direct damage to cell structure and metabolism.
Damage to cells activates markers to recruit inflammatory immune cells. These cells repair and regenerate tissue cells. They get energy from fatty acids and produce lactic acid. The result is a shift in the acid-base balance of the region. Excess acid diffuses into the local circulation and eventually is cleared by kidneys into the urine.
Urine Excretion Of Acid
The result of many regions chronically inflamed is to increase the amount of acid in urine. Enough to shift the potential of hydrogen or pH of urine, Neutral balance of pH is 7.0. Increasing acidity of urine decreases pH. Increasing alkalinity increases pH.
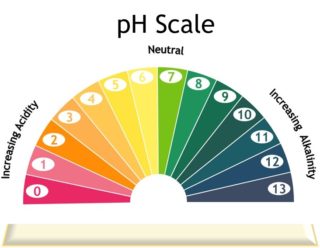 The acid-base balance of tissue fluids, blood and urine is tightly controlled. Tissue fluids and arterial blood are slightly alkaline with a pH of 7.4. After 6 to 8 hours without eating, normal pH of urine is 6.5 to 7.5. The increase in acid excretion associated with chronic inflammation causes morning urine values less than 6.0.
The acid-base balance of tissue fluids, blood and urine is tightly controlled. Tissue fluids and arterial blood are slightly alkaline with a pH of 7.4. After 6 to 8 hours without eating, normal pH of urine is 6.5 to 7.5. The increase in acid excretion associated with chronic inflammation causes morning urine values less than 6.0.
C-Reactive Protein
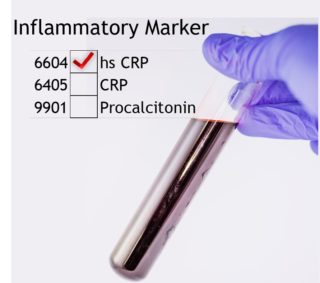 Chronic inflammation also causes an increase in high-sensitivity C-Reactive Protein.
Chronic inflammation also causes an increase in high-sensitivity C-Reactive Protein.
This protein is secreted by the liver in response to markers from damaged cells anywhere in the body. Stimulating formation of immune cells that repair and regenerate tissue.
Increased levels of this protein in blood indicate injury or infection. They also indicate inflammatory functions associated with atherosclerosis, hemorrhagic stroke and Alzheimer’s Disease.
Self-Protection From Coronavirus Infection
All along we have been expecting that vaccines will prevent COVID-19 and everything will return to what it used to be. Now we know that immunity to COVID-19 probably will have to be boosted every year or so. We also know that eventually COVID variants will require new versions of vaccine to continue preventing illness from Coronavirus infection.
Individual differences in protection from infection have been ignored. Differences in who gets infected, who gets ill, who has to be hospitalized and who won’t survive. Most people who get infected don’t even know it or don’t get seriously sick.
 Most of those ill enough to be hospitalized have poor health habits. No regular exercise, overeating, poor sleeping and continuing psychological distress. Specific genetic traits also determine who might get infected but good health habits prevent their expression. Even the response to vaccination is hurt by poor health habits.
Most of those ill enough to be hospitalized have poor health habits. No regular exercise, overeating, poor sleeping and continuing psychological distress. Specific genetic traits also determine who might get infected but good health habits prevent their expression. Even the response to vaccination is hurt by poor health habits.
Good health habits prevent Coronavirus disease and reduce its severity.
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
Sign Up