Exercise Protection from COVID Infection and Transmission
If there’s no measurable Infection, there’s no Transmission and no Illness.
Vaccination protects against severe illness but doesn’t protect against asymptomatic infection.
Exercise reduces risk of intracellular COVID infection. Works especially by restoring normal acid-base balance. That inhibits virus from entering cells. Which is important when there’s weak immune function. Weak because of immune disease, or treatment for inflammatory disease, transplant, or cancer. Weak because of disease such as hypertension, lung disease, kidney disease, diabetes or heart disease. Weak because of visceral fat or obesity. Even weak immune function just from getting older.
A weak immune system has less response to vaccination. Providing less antibody response against viral infection. Still recommended but less protection.
Not everyone exposed to COVID virus gets virus into functioning cells of lungs, heart, kidneys, muscle, fat and pancreas. Some have natural, innate full protection. Those with poor acid-base balance are poorly protected. Liable to get intracellular infection and suffer severe illness. Exercise and physical fitness restore normal acid-base balance.
Exercise and physical fitness also strengthen immune function. Even when immune function is weak.
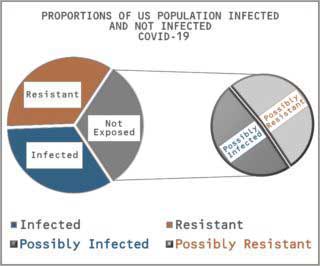 Many in the US have already been infected by SARS-CoV-2. At least one-third. Of the others, probably half haven’t yet been dangerously exposed.1
Many in the US have already been infected by SARS-CoV-2. At least one-third. Of the others, probably half haven’t yet been dangerously exposed.1
They will be. Sooner or later, everyone will be exposed. Of those not yet infected, probably half were dangerously exposed and just didn’t get infected. They were able to resist infection.
Not because they had been vaccinated against Coronavirus infection. Vaccination doesn’t prevent infection. It just prevents severe illness.
Even without symptoms of illness, people who have been infected are contagious. They expose others in close contact with them to Coronavirus infection. Any of those others who have not been vaccinated are liable to severe illness.
Not everyone exposed to SARS-CoV-2 infection gets infected. Not even when living in the same household as someone with a positive diagnosis.
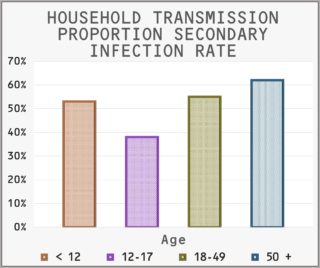 Rates of transmission have been studied in 101 households in Tennessee and Wisconsin. In each household with someone newly infected, others in the household were examined and tested repeatedly for secondarily becoming infected. During 7 days of follow-up, 54% of other members became secondarily infected. 36% were symptomatic and 18% were Infected without symptoms. 2
Rates of transmission have been studied in 101 households in Tennessee and Wisconsin. In each household with someone newly infected, others in the household were examined and tested repeatedly for secondarily becoming infected. During 7 days of follow-up, 54% of other members became secondarily infected. 36% were symptomatic and 18% were Infected without symptoms. 2
Rates of secondary infection depended on risk factors known from other clinical studies. As shown in the figure of rates in relation to age, older household members had greater rates of secondary infection than younger members.
Other risk factors such as high blood pressure, lung disease, cardiovascular disease, diabetes, obesity, and chronic inflammatory dysfunction also increase the risk of secondary infection. Studies in other clinical trials show that about half of all people everywhere have co-morbid medical conditions that increase the likelihood of becoming infected with Coronavirus.
Apparently, many people of all ages everywhere have a natural, innate resistance to Coronavirus infection. Including all the virus variants that keep appearing. What is it that protects them?
 Protection by Exercise has been studied during the COVID pandemic. Kaiser Permanente in California recorded week-by-week physical activity at outpatient health clinic visits from March 2018 to March 2020. 3
Protection by Exercise has been studied during the COVID pandemic. Kaiser Permanente in California recorded week-by-week physical activity at outpatient health clinic visits from March 2018 to March 2020. 3
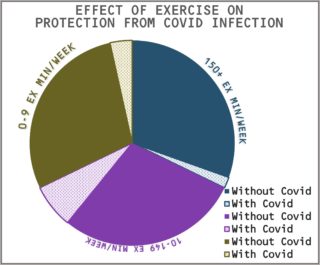
During the past 10 years, patients have been asked about their exercise. Their responses are included as vital signs in their health records. Along with body temperature, blood pressure, and pulse rate. About one-third report at least 150 minutes of moderate exercise every week. Of the others, almost one-third don’t do any exercise and the rest do less than 150 minutes.
As shown in the Figure, most of the groups with COVID infection were inconsistently active. Only 0.4% consistently exercised at least 150 minutes a week.
From January to October 2020, the clinic population of 4.7 million had about equal numbers of outpatients in each exercise group. About 2% of the total population was diagnosed with COVID-19. Those who were continuously eligible under study criteria were evaluated for risks of COVID in relation to their physical activity.
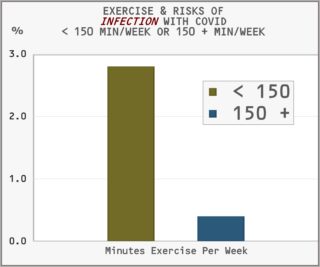

Risks of infection with COVID were much greater in those who had not been consistently active. About 3% for those who exercised less than 150 minutes a week. Less than 0.5% for those who exercised consistently at least 150 minutes a week.
Risks for severe COVID infection were much greater in those who had not been consistently active. The Figure indicates about a 20-fold increase in incidence of severe illness compared to those who had been exercising at least 150 minutes a week. Severe illness required hospitalization for 0.4% of those who had been consistently inactive. In contrast, severe illness affected only 0.02% of those who had been consistently active.
Results from other clinical studies have been similar. In addition, subjects who were older, female, belonging to minority racial or ethnic groups, were obese or had chronic health conditions were more likely to be inactive. Severity of COVID illness has always been less in subjects who consistently exercised.
Consistently, frequency and intensity of exercise are the most remarkable features discriminating between subjects at high and low risk of COVID-19 infection and severity of illness.
Energy for Action
Anything that’s alive needs energy for chemical reactions, growth, and motion. Human muscles convert chemical energy into movement with about 50% efficiency. Energy is lost in heat and CO2. Remarkably efficient considering normal body temperature is less than 100o F. A cylinder in a car engine burns fuel at 2,800o F. The result is about 10% fuel efficiency.
The breakdown of food releases energy. That energy is captured in smaller chemical forms and carried to places where energy is needed. Or places where it can be stored as carbohydrate or fat.
Protein Structure and Function
The chemical machines guiding action consist mostly of proteins bonded together. Called enzymes. Each enzyme acts on specific substances to break chemical bonds, rearrange them or make new bonds. More than 20,000 enzymes in a typical human cell.
The structure of proteins is more complex than a simple string of molecules. Strings are folded into 3-dimensional shapes. The folded proteins must be stable for enzymes to function correctly.
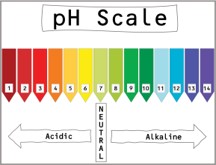
Protein folding depends on temperature and chemicals surrounding the structure. It also depends on acid-base conditions. More acidic solutions have more hydrogen positive molecules than basic solutions with more negatively charged molecules. The measure of how acidic or how basic is called pH. Which means “potential of hydrogen.” It’s a measure of how much free hydrogen carrying a positive charge is in solution.
 Optimal function depends on proteins that are fully folded. Extremes of higher or lower acid-base conditions disable normal protein function.
Optimal function depends on proteins that are fully folded. Extremes of higher or lower acid-base conditions disable normal protein function.
The range of pH goes from 0 to 14. Completely acid at 0, neutral at 7 and completely alkaline at 14.
Virus Structure and Function
A virus is a core of proteins containing genetic material surrounded by a protein capsule. It can’t capture or produce energy, move or grow. It’s not alive. It can survive and multiply only by entering living cells and capturing essential materials.
Optimal function of proteins in virus particles occurs in more acidic solutions at lower pH than optimal function of proteins in host protective enzymes.
Innate Physical and Chemical Protection
Surface skin and inside membranes keep almost everything from getting inside. Cells are arranged side by side, over and under one another. Each fastened tightly to those next to it. Injury can rip them apart. Physical force, and toxic chemicals can cause injury and some places leak enough to let things inside.
Just getting inside skin and membranes is enough for poisons and toxic chemicals to cause harm. Results of those injuries have to be taken care of.
Also, getting inside is enough for infection by bacteria, fungi, parasites and worms. They start growing and spreading. They’re alive and have to be caught and killed.
Viruses that get inside into blood and tissue juice, still can’t grow and spread. Infection is not established. They need essential materials from inside cells. Floating in fluid outside cells, they can be captured and destroyed.
Cell membranes are strong and protective. Proteins join cells together. Very few chemicals just diffuse through. Proteins control movement of chemicals in and out of the cell.
Blood, tissue and most cells are slightly alkaline. Even slight change to acid has dramatic effects. Cell protection and normal cell function depend on alkaline pH. Acidic pH causes protein structure to unfold and lose normal function. 4
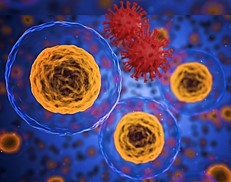 Virus infection of tissue cells depends on fusing with the cell membrane. Optimal pH for protein in a virus envelope is more acidic than protein in the host cell membrane. Alkalinity provides protection from attachment, penetration and entry of virus into cells. Once inside, the virus takes over cellular proteins that enable virus multiplication, growth and eventual destruction of the host cell.
Virus infection of tissue cells depends on fusing with the cell membrane. Optimal pH for protein in a virus envelope is more acidic than protein in the host cell membrane. Alkalinity provides protection from attachment, penetration and entry of virus into cells. Once inside, the virus takes over cellular proteins that enable virus multiplication, growth and eventual destruction of the host cell.
Natural resistance to virus infection depends on maintaining a protective acid-base balance. Slightly alkaline. Host cellular protective proteins with optimal pH higher than optimal pH for invading virus particles.
Innate Immune Protection
Cells and tissue fluid contain protein receptors that recognize patterns and structures that can cause injury. Some receptors are attached to special immune cells and some are inside normal functioning cells.
These receptors bind to anything that is not natural to the tissue. Especially dangerous foreign molecular structures. They begin the process of destroying them and activating other local immune cells.
They also signal systemic activity to bring in additional protection. Some things are captured and cleared with little local effect. More damaging substances bring out full inflammatory responses.
Cellular action that creates additional inflammatory cells and substances requires energy. That energy comes from metabolism that doesn’t require oxygen. Sugar is broken down into smaller molecules releasing energy. What’s left is lactic acid. Some of the lactic acid combines with bicarbonate and some washes away in the circulation. Either way, inflammation changes the acid-base balance in tissue and blood. More acid and less bicarbonate.
Protection from COVID Infection
The virus causing COVID circulates through droplets in the air spread by coughing or sneezing. It enters through mouth, nose or eyes and spreads to the back of the  throat. From there, it can reach the lungs. Also, it can be swallowed down to the stomach.
throat. From there, it can reach the lungs. Also, it can be swallowed down to the stomach.
Virus particles stay on the surface until breathed out or washed away. Kept out by physical and chemical barriers of the upper airway.
Protection of Nose and Throat
Captured by cilia, virus particles are bathed in secretions. Normal acid-base balance of saliva and nasal secretions varies from pH 6 to 8. 5
COVID infection of nose and throat occurs when tissue fluids become acid. Acidic pH causes cell protein structure to unfold and lose normal protective function. Virus particles fuse with protein on the cell membrane, enter the cell and take over essential protein structures. Infection is completed.
Hydration affects acid-base balance of saliva and nasal secretions. Even mild dehydration reduces rates of flow and produces acid secretions. Increased rates of flow produce secretions that are less acid and more alkaline. 6
Drinking 6 to 8 glasses of fluid a day is commonly recommended for good health. Especially with strenuous physical activity in hot or humid weather. Even more at high altitude.
Chronic, mild dehydration is a risk factor for COVID infection of nose and throat. Especially when associated with co-morbid conditions that increase risk for severe illness from COVID. Certainly, fluid intake should be at least 6 glasses a day if pH of saliva is less than 6.0. Increasing intake of fluid could well produce secretions of saliva that are less acid and reduce risk of COVID infection. 7
Rates of flow also depend on general acid-base balance in circulating blood and local tissue fluid. Any acid-base shift that reduces pH in tissue fluid reduces pH of saliva and nasal secretions.
Protection of Lungs
COVID virus moves down the airway from mouth, nose and throat to the lungs. Virus particles released from cells in the nose and throat are released into the air in droplets.
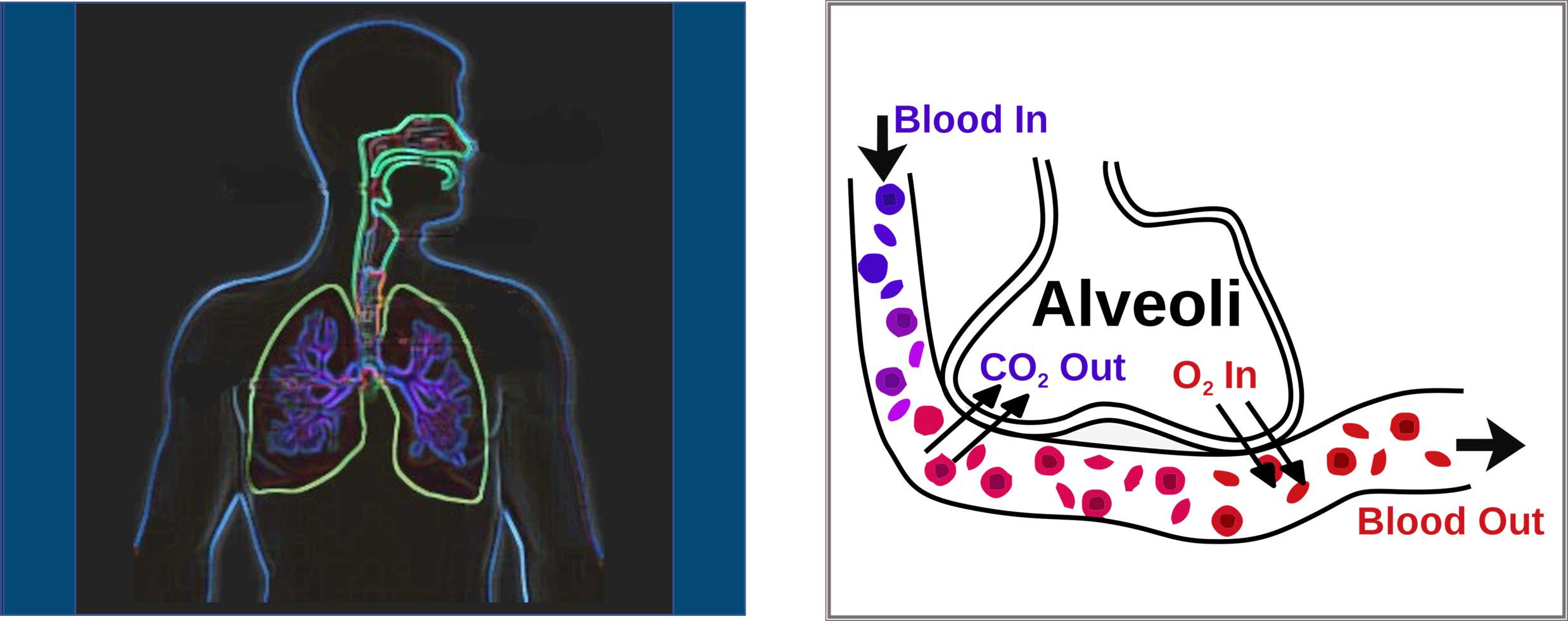
Air inhaled into the lungs fills small spaces called “alveoli.” From there, CO2 moves from blood into the air that’s exhaled. Along with droplets carrying virus particles. Most droplets carried in are carried on out. But some droplets with virus join with fluid lining the air spaces.
Dissolved in tissue fluid, CO2 is a weak acid. Released into air, it leaves behind a more basic solution. Alkaline fluid with pH greater than 6.0 effectively excludes entry of virus particles.
The acid-base balance of airway lining fluid can be measured. Droplets of fluid are caught up in exhaled air. Collected and condensed, the pH has been measured. 8
Samples of Airway Lining Fluid were collected from 404 healthy young adults living around the University of Virginia. Individuals were excluded if they had any acute or chronic condition of any system. Median pH was 8.0. Fewer 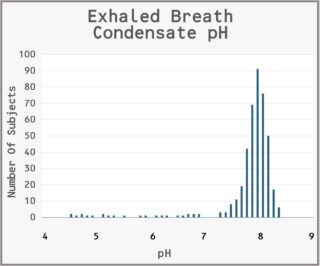 than 10% of these normal subjects had pH less than 7.4. No effect of age or sex.
than 10% of these normal subjects had pH less than 7.4. No effect of age or sex.
Release of CO2 from fluid lining air spaces in the lungs decreases acidity and increases alkalinity. Lower levels of bicarbonate and lesser loss of CO2 increase the acidity of the fluid. Increased amounts of other acids stay in the fluid and decrease the pH.
Less than 10 percent of the total quantity of carbon dioxide carried in the blood is eliminated during passage through the lungs. Slowing the flow of air out of the air spaces decreases the amount of CO2 removed. Increased concentration of CO2 in the air slows innate action to maintain and repair cells lining the air spaces.
The combination of decreased bicarbonate, increased organic acids and decreased elimination of CO2 quickly lowers the pH. Virus particles become able to fuse with cell membranes and pass into the interior. Infection is complete.
Heart Rate Response to Injury and Infection
The innate immune system includes increasing heart rate. Protein receptors that recognize danger react and send out signals for an inflammatory response. Including signals that stimulate the brain to increase heart rate. Short-term acute or long-term chronic. Complete recovery from acute injury or infection returns all systems to normal. 9 10
As a result, infection by COVID virus causes an increase in resting heart rate. Before the host has any symptoms of infection. Even before virus can be detected using a nasal swab. An alert triggered by increased heart rate forms an opportunity to isolate the newly infected host from transmitting virus to others. 11
Chronic Inflammation
Injury or infection anywhere that persists keeps resting heart rate higher than normal. Sympathetic nerves from the spinal cord act to increase heart rate. The vagus nerve, running through the neck and chest acts to slow the heart. 12
Stimulation of the vagus nerve also acts to increase secretion of saliva. Increasing not only the amount of fluid secreted but also the amount of enzymes involved in digestion. Also, the amount of immune enzymes involved in defense of salivary cells.
The defense enzymes are mostly basic proteins which increase the pH of saliva. The normal pH of saliva is about 7.0 which is neutral. At peak flow, optimum pH is close to 8.0. Much higher than optimum pH for envelope proteins of COVID viruses.
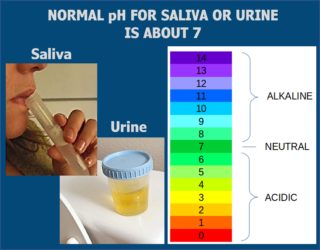
The effect of chronic inflammation anywhere enough to increase resting heart rate is to increase acidity of saliva. Decrease in pH of saliva below 6.0 increases the risk of COVID infection in the nose and throat.
Chronic inflammation also affects acid-base transport everywhere. Local action of immune cells without oxygen increases acidity of local tissues. Local tissue acidity decreases bicarbonate and increases organic acids in circulating blood. Acid-base transport in the kidneys adjusts the pH of circulating blood by excreting acid urine. Decrease in pH of urine below 6.0 increases the risk of COVID infection in the lungs.
Exercise Training for Preventing and Controlling COVID-19 Infection
Many clinical studies have shown that moderate intensity aerobic training strengthens the immune system. It’s safe and it works! Even one 10-minute session activates neural, endocrine, cellular, and humoral defense against infection. 13 14 15
Endurance training most often used is walking, running, cycling or swimming. Intensity that increases heart rate to about 70% between resting rate and maximal heart rate. Duration 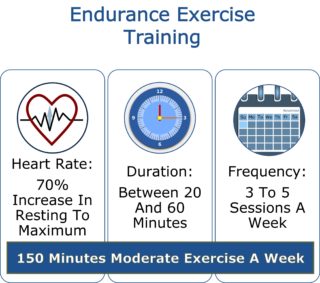 between 20 and 60 minutes. Frequency 3 to 5 sessions a week. That’s a total of moderate exercise for about 150 minutes in each week.
between 20 and 60 minutes. Frequency 3 to 5 sessions a week. That’s a total of moderate exercise for about 150 minutes in each week.
Intensity and duration for protection of most healthy people is an average heart rate between 120 and 160 bpm for at least 20 minutes. About the most that anyone can do comfortably 3 to 5 sessions a week. Able to talk but only a few words in short sentences between breaths.
So far, the best proven protective effect of regular exercise has been a lesser number of sick days. Fewer than half as many sick days in adults with exercise training over a period of 8 to 15 weeks.
The best laboratory indicator of exercise protection has been low plasma level of c-reactive protein. Levels in normal healthy adults are <3 mg/L and safest levels are <1 mg/L. CRP is produced by the liver in response to early indicators of infection and inflammation. Its level rises rapidly to a peak in about 48 hours after onset of disease. Its concentration decreases when inflammation lessens and healing begins. 16
COVID-19 infection causes average levels of 20 to 50 mg/L. Patients with severe COVID-19 requiring hospitalization had levels more than 2-fold higher than those with mild disease. Patients who died from COVID-19 had about 10-fold higher levels of CRP than the recovered patients.
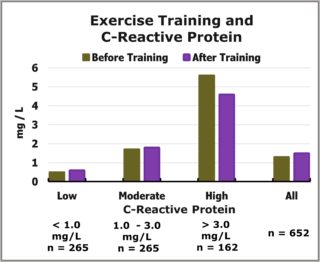 High levels of CRP in healthy adults have been measured before and after moderate exercise training. A clinical study of about 200 parents and 400 adults in their families was done in USA and Europe. About 25% of them had levels of CRP greater than 3 mg/L. Those with high levels of CRP also tended to have abnormal clinical features and other abnormal laboratory values. Many similar to individuals with hypertension, obesity, diabetes and abnormal blood lipid levels. 17
High levels of CRP in healthy adults have been measured before and after moderate exercise training. A clinical study of about 200 parents and 400 adults in their families was done in USA and Europe. About 25% of them had levels of CRP greater than 3 mg/L. Those with high levels of CRP also tended to have abnormal clinical features and other abnormal laboratory values. Many similar to individuals with hypertension, obesity, diabetes and abnormal blood lipid levels. 17
An exercise training program on cycle ergometers was conducted 3 times a week for 20 weeks. Increase in heart rate during exercise started at 55% of maximum possible during the first week and increased to 75% for the average during the last week. Maximum energy capacity increased about 18%.
Reductions in CRP only occurred in individuals with levels at baseline greater than 3 mg/L. There were no consistent associations with changes in other clinical features or laboratory values.
High levels of CRP certainly indicate high risk for severe COVID-19 illness. Whether already infected or exposed to infection. Also, moderate exercise training reduces levels of CRP in patients with comorbid conditions.
Especially evident in patients with common conditions like hypertension, lung disease, diabetes and obesity. The target of exercise training always is reducing severity of comorbid conditions.
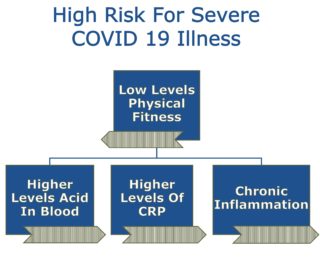 Physical fitness also affects levels of CRP and indicators of acid-base balance. Results of exercise tests were compared with blood levels measured for 2,714 healthy young adults in the US National Health and Nutrition Examination Survey (1999-2004). Lower levels of physical fitness were associated with higher levels of acid in the blood. Also, associated with higher levels of CRP. Low levels of physical fitness had chronic inflammation along with an excess of acid in tissue and blood. 18 19 20
Physical fitness also affects levels of CRP and indicators of acid-base balance. Results of exercise tests were compared with blood levels measured for 2,714 healthy young adults in the US National Health and Nutrition Examination Survey (1999-2004). Lower levels of physical fitness were associated with higher levels of acid in the blood. Also, associated with higher levels of CRP. Low levels of physical fitness had chronic inflammation along with an excess of acid in tissue and blood. 18 19 20
Apparently, physical activity including less than 15 to 30 minutes a day of moderate exercise causes the same risk to health and life as smoking tobacco.
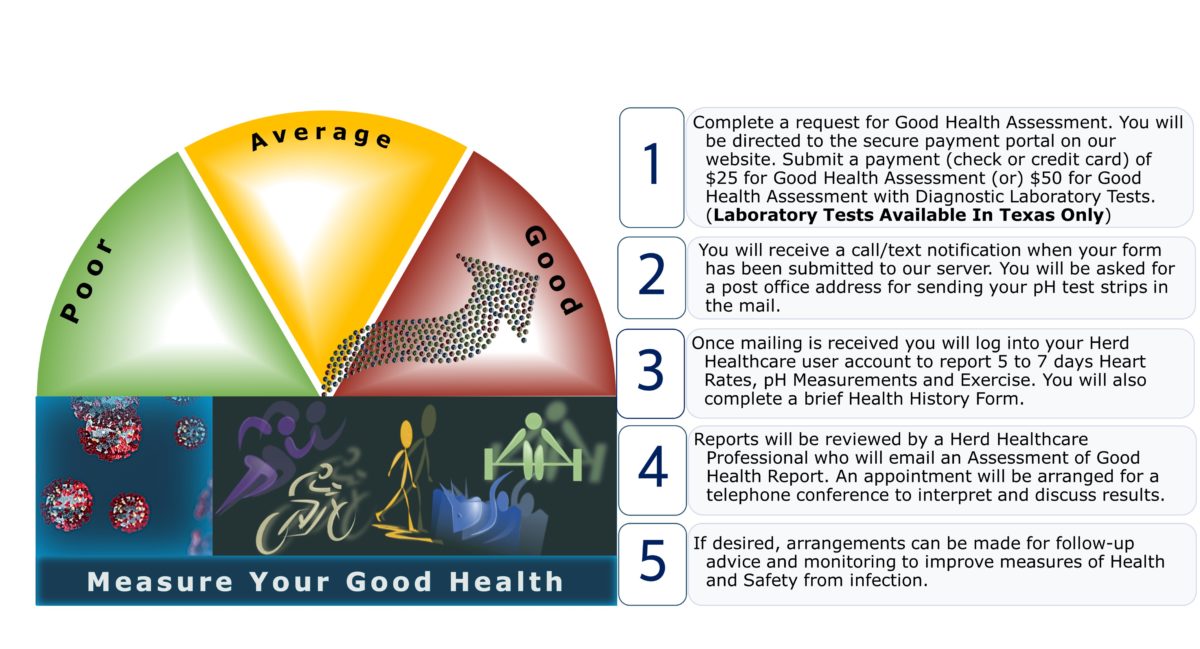
Measuring Your Good Health
Good health improves natural protection from infection. Including infection by Coronovirus-2 and variants. The strength of health-supporting protection can be evaluated by physical and laboratory tests.
Vaccines that are available provide very little protection against Coronavirus infection. They do reduce the severity of illness. At least for several months. But they do not protect against illness of all variants that continue to appear. Variants that will continue to appear as long as some people are poorly protected.
Also, protection against severity reduces but does not completely protect against transmitting infection to others.
Many people have natural features and strength of good health that reduce risk from infection. As well as risk of severe illness. Many others are in great danger of infection and illness. Almost everybody can improve their health enough to decrease risk of infection and severe illness.
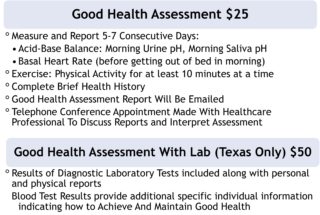 Results of laboratory tests combined with personal information can be used to determine natural features and strength of good health protecting against infection and illness.
Results of laboratory tests combined with personal information can be used to determine natural features and strength of good health protecting against infection and illness.
We will assess individual features of health to make recommendations for increasing personal safety from infection and illness.
References
1. Adams ML, Katz DL, Grandpre J. Population-Based Estimates of Chronic Conditions Affecting Risk for Complications from Coronavirus Disease, United States. Emerging Infectious Diseases. 2020;26(8):1831-1833. doi:10.3201/eid2608.200679 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7392427/pdf/20-0679.pdf
2. Grijalva CG, Rolfes MA, Zhu Y, et al. Transmission of SARS-COV-2 Infections in Households — Tennessee and Wisconsin, April–September 2020. MMWR Morb Mortal Wkly Rep 2020;69:1631–1634. doi:10.15585/mmwr.mm6944e1
https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6944e1-H.pdf
3. Sallis R, Young DR, Tartof SY, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. British Journal of Sports Medicine 2021;55:1099-1105
https://bjsm.bmj.com/content/bjsports/55/19/1099.full.pdf
4. Zhou T, Tsybovsky Y, Kwong PD. A pH-dependent switch mediates conformational masking of SARS-CoV-2 spike. bioRxiv. 2020, Jul 4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337388.1/
5. Baghizadeh Fini M. (2020). Oral saliva and COVID-19. Oral oncology, 108, 104821. doi:10.1016/j.oraloncology.2020.104821
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7250788/pdf/main.pdf
6. Stookey JD, Allu PKR, et al. Hypotheses about sub-optimal hydration in the weeks before coronavirus disease (COVID-19) as a risk factor for dying from COVID-19. Med Hypotheses. 2020;144:110237. doi:10.1016/j.mehy.2020.110237
https://www.sciencedirect.com/science/article/pii/S0306987720319460
7. Farshidfar N, Hamedani S. Hyposalivation as a potential risk for SARS-CoV-2 infection: Inhibitory role of saliva. Oral Dis. 2021;27 Suppl 3:750-751. doi:10.1111/odi.13375
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7267261/pdf/ODI-9999-na.pdf
8. Paget-Brown AO, Ngamtrakulpanit L, Smith A, et al. Normative data for pH of exhaled breath condensate. Chest. 2006;129(2):426-430. doi:10.1378/chest.129.2.426
https://www.researchgate.net/publication/7297871_Normative_Data_for_pH_of_Exhaled_Breath_Condensate
9. Whelton SP, Narla V, Blaha MJ, et al. Association between resting heart rate and inflammatory biomarkers (high-sensitivity C-reactive protein, interleukin-6, and fibrinogen) (from the Multi-Ethnic Study of Atherosclerosis). Am J Cardiol. 2014;113(4):644-649. doi:10.1016/j.amjcard.2013.11.009
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4280910/pdf/nihms651029.pdf
10. Sajadieh A, Nielsen OW, Rasmussen V, et al. Increased heart rate and reduced heart-rate variability are associated with subclinical inflammation in middle-aged and elderly subjects with no apparent heart disease. Eur Heart J. 2004;25(5):363-370. doi:10.1016/j.ehj.2003.12.003
https://academic.oup.com/eurheartj/article/25/5/363/485118
11. Hirten RP, Danieletto M, Tomalin L, et al. Use of Physiological Data From a Wearable Device to Identify SARS-CoV-2 Infection and Symptoms and Predict COVID-19 Diagnosis: Observational Study. J Med Internet Res. 2021 Feb 22;23(2):e26107. doi:10.2196/26107
https://www.jmir.org/2021/2/e26107/PDF
12. Farwell WR, Taylor EN. Serum anion gap, bicarbonate and biomarkers of inflammation in healthy individuals in a national survey. CMAJ. 2010;182(2):137-141. doi:10.1503/cmaj.090329
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2817320/pdf/1820137.pdf
13. Scudiero O, Lombardo B, Brancaccio M, et al. Exercise, Immune System, Nutrition, Respiratory and Cardiovascular Diseases during COVID-19: A Complex Combination. Int J Environ Res Public Health. 2021;18(3):904. Published 2021 Jan 21. doi:10.3390/ijerph18030904
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7908487/pdf/ijerph-18-00904.pdf
14. Hilde Grindvik Nielsen (May 15th 2013). Exercise and Immunity, Current Issues in Sports and Exercise Medicine, Michael Hamlin, Nick Draper and Yaso Kathiravel, IntechOpen, DOI: 10.5772/54681. Available from:
https://www.intechopen.com/chapters/44616
15. Stewart LK, Flynn MG, Campbell WW, Talbert E, et al. The influence of exercise training on inflammatory cytokines and C-reactive protein. Med Sci Sports Exerc. 2007;39(10):1714-1719. doi:10.1249/mss.0b013e31811ece1c
16. Martins RA, Veríssimo MT, et al. Effects of aerobic and strength-based training on metabolic health indicators in older adults. Lipids Health Dis. 2010;9:76. Published 2010 Jul 22. doi:10.1186/1476-511X-9-76
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2912308/pdf/1476-511X-9-76.pdf
17. Lakka TA, Lakka HM, Rankinen T, et al. Effect of exercise training on plasma levels of C-reactive protein in healthy adults: the HERITAGE Family Study. Eur Heart J. 2005;26(19):2018-2025. doi:10.1093/eurheartj/ehi394
https://academic.oup.com/eurheartj/article/26/19/2018/532081
18. Abramowitz MK, Hostetter TH, Melamed ML. Lower serum bicarbonate and a higher anion gap are associated with lower cardiorespiratory fitness in young adults. Kidney Int. 2012;81(10):1033-1042. doi:10.1038/ki.2011.479
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3340439/pdf/nihms346734.pdf
19. Aeschbacher S, Schoen T, Dörig L, et al. Heart rate, heart rate variability and inflammatory biomarkers among young and healthy adults. Ann Med. 2017;49(1):32-41. doi:10.1080/07853890.2016.1226512
https://www.tandfonline.com/doi/pdf/10.1080/07853890.2016.1226512?needAccess=true
20. Farwell WR, Taylor EN. Serum anion gap, bicarbonate and biomarkers of inflammation in healthy individuals in a national survey. CMAJ. 2010;182(2):137-141. doi:10.1503/cmaj.090329
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2817320/pdf/1820137.pdf





