Telehealth Reduce Employee Healthcare Costs of COVID-19
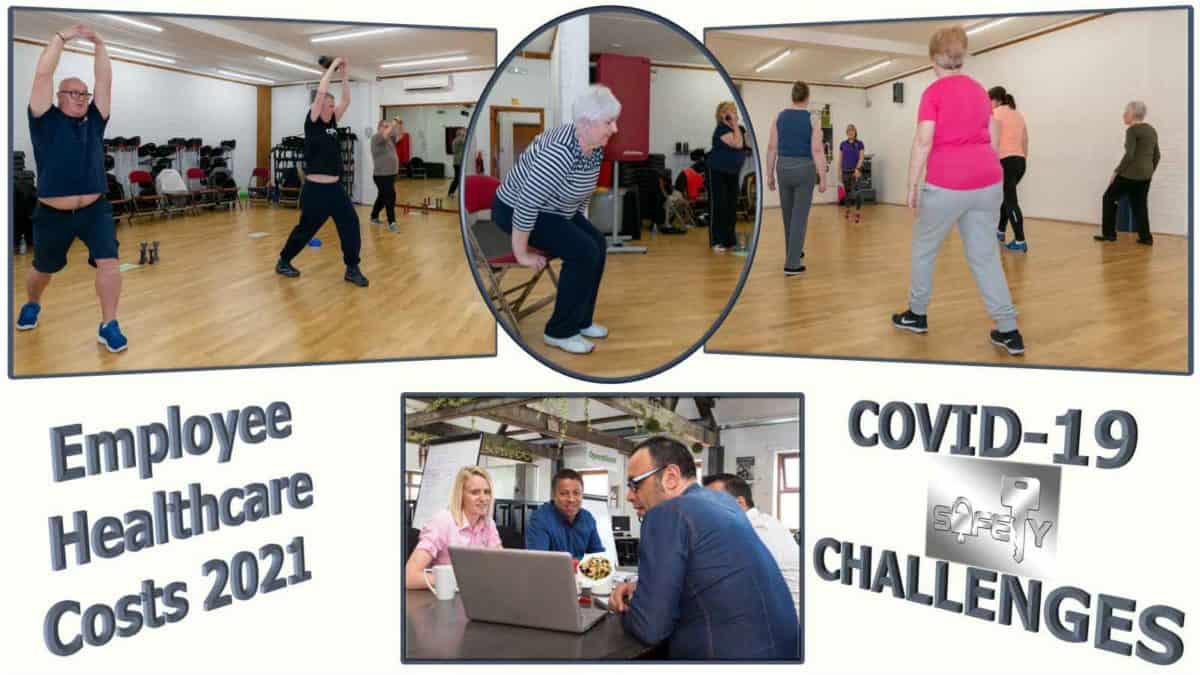
Healthcare is always our biggest expense! Job losses during COVID-19 threaten Employer-sponsored health insurance. Which is about 34% of healthcare expenses.
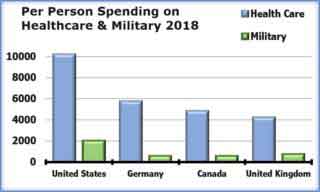
About an equal amount is paid by public funds – Medicare (20%) and Medicaid (17%). The rest of healthcare costs are paid by Donations (19%) and Out-of-pocket expenses (10%). Each year, we spend more because of poor health than we spend on the military and national security.
To learn more about programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
Healthcare for Business and Industry
Employer-sponsored healthcare began during World War II. The Stabilization Act of 1942 limited wage increases. To attract new employees, US businesses used employer-sponsored health insurance. Employees didn’t have to pay taxes on sponsored healthcare and they got coverage for themselves and their families.
Other types of benefits included Life insurance, Retirement plans and Disability insurance. Medical insurance was the most popular.
Since then, employer-sponsored healthcare has increased. Initially, only large corporations were self-insured and implemented their own  insurance plans. Especially in industries where employees had a high risk of injury.
insurance plans. Especially in industries where employees had a high risk of injury.
Now, increasing costs of healthcare and changes in healthcare regulations have caused small and medium-sized businesses to become self-insured. Along with opportunities and incentives to reduce healthcare costs.
Designing and implementing healthcare programs for business and industry has become an industry of “Professional Employer Organizations.”
Employee Health Benefits
Most large US employers offer a health-contingent program as part of their employees’ health benefits. These support employees in making changes to health behaviors. Including changes to reduce risk for certain chronic medical conditions and manage them more effectively.
They include health screening for risk factors as well as education and coaching for cessation of tobacco use, promotion of physical activity, stress reduction, and weight management. Some programs also include chronic disease management.
Most large employers ask for personal health information. The majority use a health risk assessment (HRA) questionnaire and some use  screening by a physical examination or lab test. In addition, some large employers collect information through wearable technologies. Approximately a third of large firms offer incentives to disclose health information.
screening by a physical examination or lab test. In addition, some large employers collect information through wearable technologies. Approximately a third of large firms offer incentives to disclose health information.
A small percent also offer incentives to reduce body weight or improve blood cholesterol levels. These health-contingent wellness programs were authorized first in 2006, and later by the Affordable Care Act.
Randomized Controlled Clinical Trials
The health, economic and employment effects of education and coaching have been studied in the US. Effects  of health and wellness programs in 20 worksites were compared with health, economic and employment outcomes for 20 worksites without health-contingent programs. Each group included about 4,000 employees.
of health and wellness programs in 20 worksites were compared with health, economic and employment outcomes for 20 worksites without health-contingent programs. Each group included about 4,000 employees.
Over an 18-month period, programs offered at treatment worksites included 8 sequentially delivered sessions instructed by dietitians, each of 4 to 7 weeks in duration. Approximately 35.2% of employees in the treatment worksites completed at least 1 set of education and coaching sessions.
After 18 months, 29% of employees in the untreated groups had high cholesterol, 23% had hypertension, and 43% were obese. No statistically significant differences were detected between the employees in the untreated group worksites and treatment group worksites. Also, there were no significant differences in mean medical care spending or utilization.
Data from all worksites were examined to determine absenteeism, job tenure, and performance review scores. Here again, there were no significant differences in productivity or performance between employees in the treated and untreated worksites.
Financial Incentives
In 1996, the Health Insurance Portability and Accountability Act (HIPAA), allowed financial incentives for programs of health promotion and disease prevention. Initial limit was 20% of total healthcare coverage. In 2010, the Affordable Care Act lifted the ceiling on health-contingent program incentives to 30 percent. This limit was close to $1,800 annually for an average employee-only plan.
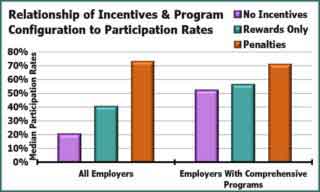 Employers offering health and wellness programs frequently include monetary incentives to encourage participation. Surveys show incentives are associated with higher participation rates. Especially in larger firms with comprehensive programs. They have the highest participation rates. Access to a more expensive plan elicits a participation rate of 40%. Incentives structured as penalties for not participating have an even higher participation rate of 73%.
Employers offering health and wellness programs frequently include monetary incentives to encourage participation. Surveys show incentives are associated with higher participation rates. Especially in larger firms with comprehensive programs. They have the highest participation rates. Access to a more expensive plan elicits a participation rate of 40%. Incentives structured as penalties for not participating have an even higher participation rate of 73%.
Chronic conditions are the major cause of illness, disability, and death in the United States. A RAND Wellness  Programs Study showed 87% of participants in worksite wellness programs had risk factors for costly disease. Only 13% had chronic disease requiring daily management.
Programs Study showed 87% of participants in worksite wellness programs had risk factors for costly disease. Only 13% had chronic disease requiring daily management.
Savings in healthcare costs resulted from about $30 per participating 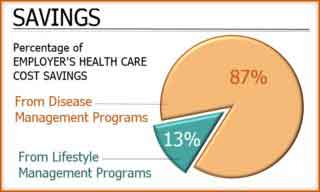 employee per month. This reduction was caused almost entirely by a 30% reduction in hospital admissions among 13% of employees who had chronic conditions. Most of the reduction in hospital admissions was the result of improved disease management.
employee per month. This reduction was caused almost entirely by a 30% reduction in hospital admissions among 13% of employees who had chronic conditions. Most of the reduction in hospital admissions was the result of improved disease management.
In 2010, the Affordable Care Act allowed incentives for health outcomes up to 30% of the cost of the group health plan. However, few employers offer this type of health program. In 2019, only 7% of large employers offered health-contingent wellness programs.
Coronavirus Infection, Symptoms and Severe Illness
COVID-19 is a viral infection that spreads from person to person. It surely started in animals but it spreads in people. Everywhere as fast and as far as an airplane can fly. What can we do?
We hear the most instruction about using public health and social measures. Actions by individuals, communities, governments and travel that slow down spread. What else can we do? Each of us can improve our health enough to prevent getting really sick.
The best sources of information report that about 25% of people in the US already have been infected by COVID-19. About a third of those infected didn’t even know it and another third had minor symptoms. Others became so ill they had to be hospitalized and one or two percent died.
Many of those who became seriously ill were already sick with heart disease, lung disease or diabetes. But the biggest group of seriously ill were simply overweight or obese. Especially high % body fat with visceral obesity. Something that can be prevented, recognized, measured, and corrected.
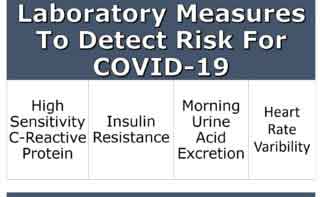 All are indicators of Subcutaneous Adipopenia and Chronic Inflammation.
All are indicators of Subcutaneous Adipopenia and Chronic Inflammation.
All are avoidable, measurable and correctable in a corporate health program.
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
Sign Up