Telehealth Reverse Diabetes With Low Basal Heart Rate | Free Trial in TEXAS
Basal heart rate is absolutely the best predictor of chronic disease, disability and premature death.
A difference of 10 bpm indicates 10% more or less risk of poor health. Above 70 bpm predicts average to awful. Less than 60 bpm indicates good to superb.
Moderate physical activity and calorie restraint make a difference. Just be sure to check your plans with your personal physician.
Sign UpTo learn more about programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
Measuring Basal Heart Rate
Heart Rate is the number of times the heart beats every minute. Specialized cells in pacing regions of the heart keep the heart beating no matter what. Additional control comes from metabolism, neural stimulation and circulating hormones.
Things happen all day that affect control of heart rate. The fewest minute to minute changes from outside the heart happen during sleep. That rhythm while sleeping is Basal Heart Rate.
The best time to measure Basal Heart Rate is immediately after waking up. Even before getting out of bed to go to the bathroom. Later in the day, Resting Heart Rate can be measured after 10 minutes of lying down comfortably in a quiet room, eyes closed and undisturbed by light, sound or movement. But it’s never quite the same as during sleep.
During the day, heart rate is affected by hydration, food, caffeine, alcohol, physical activity, hunger, posture, ambient temperature, emotions and anxiety, psychological stress and alertness. Conditions are never the same as just after several hours of sleep.
If you want to know basal heart rate and whether something is affecting health, measure basal heart rate 5 mornings in a row and calculate the average. After 3 weeks, do it again and compare the average values. A difference of 10 bpm indicates 10% improvement or regression in state of health.
Significance Of Basal Heart Rate
Normal Range for Resting Heart Rate (RHR) changes slightly with age. As shown in the Figure, average values are between 70 and 75 bpm.
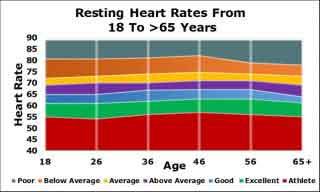 People at any age with RHR above 80 bpm have poor health and a poor outlook for disease, disability and premature death.
People at any age with RHR above 80 bpm have poor health and a poor outlook for disease, disability and premature death.
In contrast, people with RHR below 65 bpm have expectations for continued good health.
Basal Heart Rate is associated with Metabolic Syndrome, Type 2 Diabetes, Heart Disease, Stroke, Cancer, Dementia, Depression and Anxiety.
Mortality and Resting Heart Rate (RHR) has been studied. Results were reported for 798 men in Sweden who were 50 years of age when recruited. Examinations were done several times during the next 21 years.
Men with RHR over 75 beats per minute at 50 years of age had twice as high risk of all-cause death, cardiovascular disease and coronary heart disease during 21 years of follow-up compared with men with RHR of 55 beats per minute or below.
The relative risk with 10 beats/min increase of resting heart rate was +9% for all-cause mortality and +8% for cardiovascular mortality.
Compared with 45 beats/min, the risk of all-cause mortality increased significantly with increasing RHR. A significantly increased risk of cardiovascular mortality was seen at 90 beats/min.
Risk for Type 2 Diabetes also has been studied. A large cohort of 73,357 people in Asia was studied for 4 years. None of the participants had diabetes at the time of recruitment into the study.
During the next 4 years, 24% of the people developed prediabetes 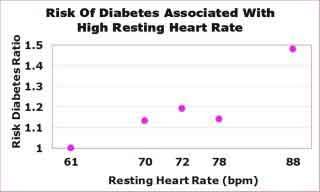 and 6% developed diabetes.
and 6% developed diabetes.
The Figure shows that the top 20% of people who had the highest average RHR of 88 bpm had almost 50% more diabetes than the lowest 20% of people who had RHR of 61 bpm.
Features Associated With Resting Heart Rate (RHR)
Physical Fitness is strongly related to RHR. Furthermore, both physical fitness and RHR are related to Mortality.
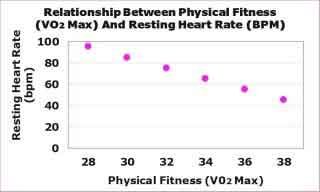 A total of 2,790 subjects in Denmark were followed for 16 years. As shown in the Figure, physical fitness was inversely related to RHR. Assessment of physical fitness included measurement of maximum oxygen consumption during graded exercise tolerance test.
A total of 2,790 subjects in Denmark were followed for 16 years. As shown in the Figure, physical fitness was inversely related to RHR. Assessment of physical fitness included measurement of maximum oxygen consumption during graded exercise tolerance test.
Both physical fitness and RHR were strongly related to mortality. However, statistical analysis demonstrated that RHR also had an independent relation to mortality.
Insulin Resistance also is strongly related to RHR. Both insulin resistance and resting heart rate are associated with increased sympathetic nervous system activity. Therefore, it is not surprising that Increased Insulin Resistance is associated with Increased Resting Heart Rate.
A population of 460 patients in 4 US communities were examined for Insulin Resistance, Resting Heart Rate and Waist Circumference. All of them had moderate kidney disease.
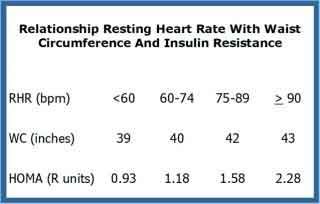 The subjects were divided into 4 groups according to Resting Heart Rate. Insulin Resistance was calculated from values for insulin and glucose measured in blood collected during fasting.
The subjects were divided into 4 groups according to Resting Heart Rate. Insulin Resistance was calculated from values for insulin and glucose measured in blood collected during fasting.
As can be seen in the Table, subjects with RHR greater than 90 bpm had more than twice the level of Insulin Resistance as those with RHR less than 60 bpm.
These data do not indicate whether RHR was caused by Insulin Resistance or excess visceral fat. It also is possible that both RHR and Insulin Resistance were caused by increased Sympathetic Nervous System Activity.
Whatever the cause for increased Resting Heart Rate, it all probably begins with excess toxic levels of sugar and fat in the blood. Excess simply can’t be cleared into glycogen and triglyceride stores in muscle and liver. The end result is increased Sympathetic Nervous System activity and increased Basal Heart Rate.
Managing Basal Heart Rate
Moderate physical activity and calorie restraint are basic principles of good health for everybody. How much physical activity and which nutrients to add or restrict must be discussed with your personal physician.
Heart and blood vessel disease, kidney disease, joint disease and gastrointestinal disease all have to be taken care of in special ways. If you’re injecting insulin or other medication to control blood sugar, you must balance exercise, calorie intake and medication. If you’re increasing intake of protein, your kidneys must handle added waste products from protein metabolism. Everything must be checked out before you make big changes in nutrition and physical activity.
An Exercise Stress Test gives good information for everybody. It provides a baseline for exercise training. It shows how much your muscles and joints will tolerate. It reveals limits of exertion for your heart and blood vessels you and your doctor might not know about.
Most people don’t need an Exercise Stress Test before they start exercise training. However, it is essential for some people. Just be sure to ask your personal physician for advice what to do.
Exercise Training is the most direct way to lower Basal Heart Rate. A consistent regular exercise training program can decrease Basal Heart Rate in 2 or 3 weeks.
All types of exercise training have been studied and a review of 191 studies has been published. These studies included 12,953 individuals in treatment and 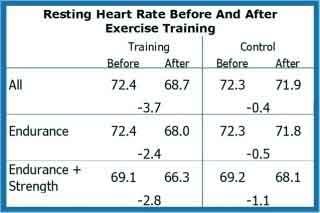 control groups. Types of exercise included 121 endurance training, 43 strength training, 15 combined training and the rest were assortments of various strenuous physical activities. Subjects exercised an average of 3 times per week during 2 weeks to 2 years.
control groups. Types of exercise included 121 endurance training, 43 strength training, 15 combined training and the rest were assortments of various strenuous physical activities. Subjects exercised an average of 3 times per week during 2 weeks to 2 years.
As shown in the Table, only endurance training significantly decreased the RHR in both sexes. The combination of endurance and strength training did not improve results.
Calorie restriction reverses sympathetic nervous stimulation of the heart and lowers Basal Heart Rate. Results from a clinical study of 22 men and women in the US, Canada and the UK who followed Caloric Restriction (CR) to about 1,800 kcal/day were compared to 20 age-related men and women in the US who consumed an ordinary Western Diet (WD) about 2,500 kcal/day.
Average nighttime Heart Rate while sleeping was 50 bpm in CR subjects compared to nighttime HR of 81 bpm in WD subjects. Total body fat in CR subjects was 9.9% compared to 24.3% in WD subjects.
Reversing Diabetes decreases cardiovascular risk factors including Resting Heart Rate. A clinical trial in Italy assigned 74 individuals with type 2 diabetes to hypocaloric diet or unchanged diet for 6 months.
Patients in the treatment group had significant reductions in severity of diabetes but none completely reversed their diabetes. However, patients in the treatment group had significantly greater reductions in Resting Heart Rate than patients in the control group.
Summary
High Basal Heart Rate is an indicator of chronic disease. The condition most commonly associated with high Basal Heart Rate is Metabolic Syndrome which forecasts Type 2 Diabetes.
The most effective way to reduce Basal Heart Rate is Exercise Training.
Calorie restriction which reduces % Body Fat also reduces Basal Heart Rate.
We can help you measure and evaluate your Basal Heart Rate and help you implement a plan to manage functions that control it.
 We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com