Telehealth Diabetes Reversal And Increase Energy Efficiency | Free Trial In Texas
Nutrigenetics and thermic effects of insulin determine the response to diet and exercise.
Normal human function depends on keeping brain temperature between 98° and 100° F.
Brain function generates considerable heat and cerebral blood flow cools it back down. As long as blood sugar levels are between 70 and 130 mg/dL there’s plenty of fuel to keep brain temperature steady at 99° F.
Sign UpTo learn more about the programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
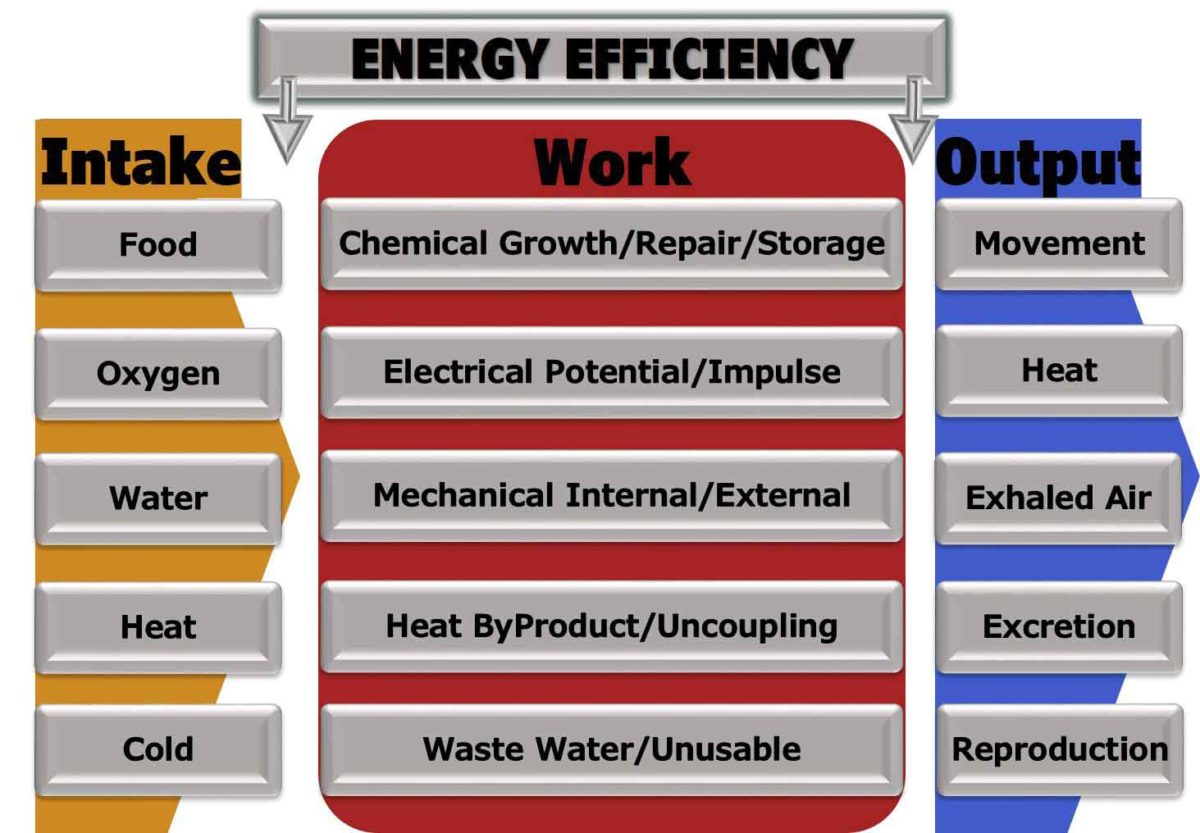
Energy Efficiency of Metabolism
We are warm-blooded creatures and our performance depends on keeping core body temperature in a narrow range. Brain temperature accounts for about 20% of the total oxygen consumption at rest.
Brain metabolism for cell maintenance, growth, repair and removal takes about 50% of the energy provided in glucose extracted from blood. The other half is heat. Some is held to maintain temperature for optimal function. The rest is released into cerebral venous blood.
There’s no energy stored in brain tissue. Electrical gradients and spikes of activity are transformed almost entirely to heat. Impaired memory starts when brain temperature falls below 98° F and impaired neuronal activity starts when brain temperature rises above 101° F. Controlling temperature of the body and maintaining a supply of glucose in blood depends on chemical, electrical and mechanical work performed in the rest of the body.
Core Body Temperature is the result of heat produced by all organs and tissues. The site that most reliably represents Core Body Temperature is in the pulmonary artery. Average normal Core Body Temperature is 98° F. Oral temperature is about -0.25° F lower.
 The heat in blood brought to the pulmonary artery is distributed throughout the body including the skin. Blood temperature at the skin is increased or decreased by exchange with the air around and can be cooled by sweating.
The heat in blood brought to the pulmonary artery is distributed throughout the body including the skin. Blood temperature at the skin is increased or decreased by exchange with the air around and can be cooled by sweating.
Under normal conditions of nutrition, there’s plenty of chemical energy in sugar, fat and proteins brought in blood circulated to organs and tissues throughout the body. Also, under normal conditions of respiration and ambient air, there’s plenty of oxygen available for metabolism to use, transfer and store energy.
The critical control is temperature of organs and tissues. Temperature has to be just right for optimal function.
Work Performed requires energy. Greatest amounts of energy are required by brain, liver, heart and kidneys. When active, skeletal muscle also requires a lot of energy.
All the chemical, electrical and mechanical work effectively applies less than half of the energy brought to organs and tissues. Approximately 40% under normal conditions of nutrition, environment and good health. Metabolism is not completely efficient and heat is produced while chemical, electrical and mechanical work is going on. What’s not used is released as carbon dioxide and heat.
That heat is not wasted. It’s distributed in blood circulating throughout the body in volumes adjusted to maintain ideal local temperatures.
Thermic Effect of Food is the amount of energy above basal metabolic rate that is required to process food for use and storage. It’s the energy required for enzymatic reactions to break food down into units that can be absorbed into blood and distributed throughout the body. The amount of energy required is about 10% of the total energy extracted from food digested, absorbed and distributed.
The thermic requirements for some types of food require more energy than others. Undigestible fiber burns energy by enzymatic reactions attempting to break it down. Mixed food that is unprocessed burns calories by reactions separating out complex proteins, fats and starches before reducing them to simple sugars, fatty acids and protein molecules that can be absorbed.
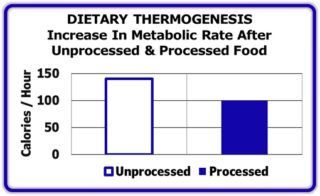 As shown in the Figure, Unprocessed food burns 40% more calories while being absorbed than Processed foods. The result for an obese individual is more excess calories from food eaten that will be stored as fat that worsens obesity.
As shown in the Figure, Unprocessed food burns 40% more calories while being absorbed than Processed foods. The result for an obese individual is more excess calories from food eaten that will be stored as fat that worsens obesity.
Dietary-Induced Thermogenesis often is used to describe Thermic Effect of Food. In fact it includes more than the energy cost of digesting and absorbing food from the gastrointestinal tract. It also includes effects of hormonal, neurogenic, chemical and enzymatic processes that affect the energy cost of transforming carbohydrates, fats and proteins into energy laden molecules that enable work.
Basal Metabolic Rate requires about 60% of Total Energy Expenditure (TEE) during 24 hours. As a rough average, energy efficiency is about 40%. That means that 24% of the TEE actually produces chemical, electrical and mechanical work. The other 76% is released as heat.
Physical Activity requires about 20% of TEE. Again, as a rough average, active skeletal muscle has an energy efficiency of about 50%. That means that half of the energy consumed by active skeletal muscle actually produces mechanical work. That also means another 10% of TEE is applied for work and 10% released as heat.
Non-shivering Thermogenesis is diet-induced heat production by the Autonomic Nervous System. This is a metabolic process located primarily in brown adipose tissue. It requires about 10% of TEE.
Epigenetic Energy Efficiency Response to Dietary-Induced Thermogenesis (DIT). This is highly individual. For example, lean people have greater energy requirements from DIT than obese people. Also, underfeeding food requires less energy for DIT than overfeeding.
It is controlled by epigenetic functions governing gene expression. Partly these are inheritable and partly they are changeable by repetitious behavior during growth, development, maturation and aging.
Potential Range of TEE affecting Energy Efficiency of DIT includes:
• Thermic Effect of Food 10%
• Energy Expenditure of Metabolism 15%
• Skeletal Muscle Efficiency 10%
• Non-Shivering Thermogenesis 10%
• Core Body Temperature (1° F) 5%
That’s a Range up to 50% of TEE! It is possible for an obese adult to adapt to caloric restriction of 50% without change in Body Weight.
Metabolic Response to Caloric Restriction
Successful weight loss for obese adults varies a great deal between individuals. Body weight of an obese adult may not change at all if Caloric Restriction is less than 50%. Even with Caloric Restriction of 50%, some obese adults may lose more than -10% Body Weight in 6 weeks while others may lose less than -5%.
Loss in body weight of at least -10% brings a reduction in Total Energy Expenditure (TEE) during 24 hours of about -15%. More than what would be predicted from changes in body composition. Those who lose less body weight have less change in TEE. Consequently, the same Caloric Restriction for all subjects caused a range of reduction in TEE that varies by about 50%.
This individual variation in Metabolic Response to Caloric Restriction was 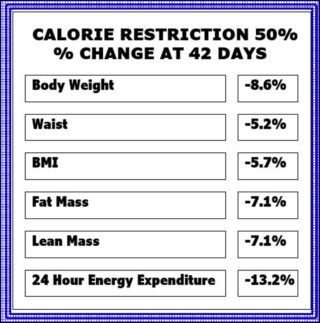 demonstrated in 47 obese men and women in Arizona. All were studied during a weight maintaining period, fasting, overfeeding and 6 weeks of 50% Caloric Restriction. The Table shows the % change in measurements after 6 weeks of Caloric Restriction. Note that there was equal loss of Fat Mass and Lean Mass. However, there was a reduction in Waist Circumference indicating a substantial reduction in Visceral Fat Mass.
demonstrated in 47 obese men and women in Arizona. All were studied during a weight maintaining period, fasting, overfeeding and 6 weeks of 50% Caloric Restriction. The Table shows the % change in measurements after 6 weeks of Caloric Restriction. Note that there was equal loss of Fat Mass and Lean Mass. However, there was a reduction in Waist Circumference indicating a substantial reduction in Visceral Fat Mass.
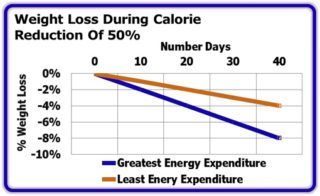 The Figure shows the % Weight Loss of two groups during 6 weeks of Caloric Restriction. The top line is the average value for 6 with the least change in Body Weight and the bottom line is the average value for 6 who had the greatest change. Note that the top line has half the slope of the bottom line.
The Figure shows the % Weight Loss of two groups during 6 weeks of Caloric Restriction. The top line is the average value for 6 with the least change in Body Weight and the bottom line is the average value for 6 who had the greatest change. Note that the top line has half the slope of the bottom line.
Autonomic Nervous System Response to Caloric Restriction
The Autonomic Nervous System (ANS) regulates Cardiovascular Function and Energy Expenditure (EE).
Basal Heart Rate upon awakening first thing in the morning is a good index of ANS function. It indicates, particularly, the stimulating effects of the ANS on both the Circulation and the Basal Metabolic Rate (BMR).
Caloric Restriction for 6 months has an effect to reduce Total Energy Expenditure (TEE) during 24 hours as well as reduce the BMR. Regular Daily Exercise increases ANS stimulation of Heart Rate and Metabolic Rate during exercise. However, between exercise sessions, the ANS decreases HR and BMR.
These interactions between ANS, TEE and HR were studied for 6 months in 28 Overweight men and women in Louisiana. Of these subjects, 7 were maintained in a Control Group, 13 were fed a caloric restricted -25% diet and 8 were fed a caloric restricted -12.5% diet and exercised daily to reduce caloric balance an additional -12.5%.
The Table shows the effects on Body Weight, Body Composition and Basal Heart 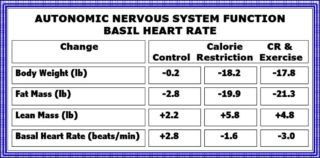 Rate. Both groups in negative caloric balance decreased their weight of Fat about 20 lb and both increased their Lean weight about 5 Lb. Also, both intervention groups had a reduced Basal Heart Rate.
Rate. Both groups in negative caloric balance decreased their weight of Fat about 20 lb and both increased their Lean weight about 5 Lb. Also, both intervention groups had a reduced Basal Heart Rate.
These results indicate that ANS reduced stimulation of Basal Heart Rate during Caloric Restriction.
Core Body Temperature During Caloric Restriction
Caloric restriction inevitably lowers Basal Metabolic Rate. With less heat generated by organs and tissues, blood circulating back to the heart contains less heat.
Adjustments by the Autonomic Nervous System (ANS) increase the production of heat by brown adipose tissue and decrease the volume of blood that can be cooled by flowing through blood vessels in the skin. Hormones secreted by the ANS also decrease the effect of insulin clearing glucose from blood. The initial result of these adjustments is to decrease heat loss.
Dietary-Induced Thermogenesis (DIT) opposes the effects of ANS during caloric restriction but with great individual variation. Some individuals with little effect on DIT will have increased HR and maintain Core Body Temperature (CBT).
Sustained Caloric Restriction for as long as 6 months induces adjustments in DIT that reduce Core Body Temperature. These results were demonstrated in 48 men and women during normal daily life in the U.S. Caloric intake was -23% lower in 24 subjects while 24 consumed a usual Western Diet.
The Table shows that CBT was lower in those subjects consuming less calories. 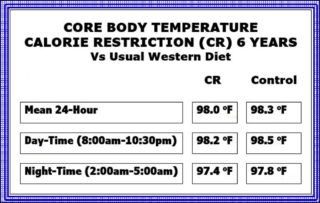 The difference was particularly evident during the night-time hours. Also, those with the greater body fat had the lowest CBT.
The difference was particularly evident during the night-time hours. Also, those with the greater body fat had the lowest CBT.
Other studies have confirmed that Obese individuals have greater adjustments in DIT during Caloric Restriction to conserve Body Weight than individuals who are Overweight or Normal in Weight.
Resistance Strength Training
Resting Energy Expenditure is reduced in older adults. Studies show that’s caused by decreased Fat-Free Mass and increased Fat Mass. Resistance Strength Training is the way to fix all that. Progressive Resistance Training increases Total Energy Expenditure and improves Insulin Sensitivity. Even without losing Body Weight.
These results were demonstrated in 9 men in Europe who were 60 to 70 years old. They all had Type 2 Diabetes and were sedentary and untrained in regular exercise. All were examined for caloric intake, body composition, strength, and metabolic variables including fasting blood glucose, HbA1c and insulin sensitivity.
Physical exercise training was done two times each week for 16 weeks. Each session was 45 to 60 minutes of progressive resistance exercise for upper, lower and core body muscle groups. All obtained greater than 10% increase in muscle strength.
 The Table shows data for Resting Metabolic Rate and Body Composition.
The Table shows data for Resting Metabolic Rate and Body Composition.
Results were favorable. Resting Metabolic Rate and Lean Body Mass increased while Fat Mass decreased. Total Abdominal Fat was decreased and Insulin Sensitivity was increased. There was no change in body Weight.
Summary
The lack of metabolic response to Caloric Restriction and plateau of Body Weight is an indication to increase protein intake (if good renal function) and implement a Resistance Strength Training Program to increase Energy Efficiency.
 We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com