Telehealth Reverse Diabetes and Maintain Remission | Free Trial In Texas
A good start reversing diabetes makes all the difference. Remission in the first 8 months is a good indicator of what to expect after 8 years.
Removing fat from muscle and liver decreases insulin resistance. Removing fat from pancreas increases secretion of insulin.
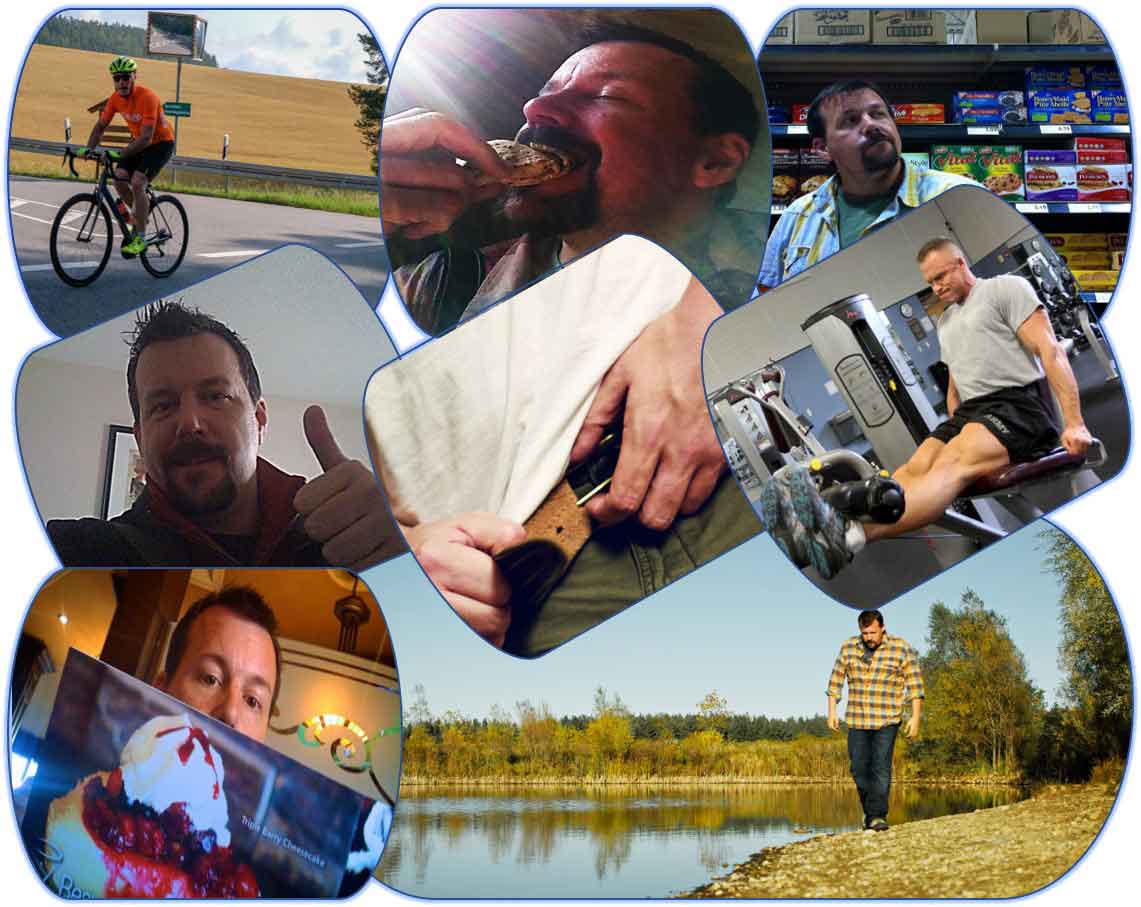
Both strenuous exercise training and severe calorie restriction remove fat from muscle, liver and pancreas. Improved insulin secretion and decreased insulin resistance maintain remission and prevent return of glucose intolerance.
Sign UpLet us help you get that good start.
To learn more about programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
Reversing Type 2 Diabetes
Diabetes mellitus creates a level of sugar and fat in the blood that is more than is healthy. The increased level causes damage to organs during the short term and disabling chronic diseases during the long term. Clearing sugar and fat from the blood involves using sugar and fat for energy needed immediately and storing the extra in muscles, liver and fat until it’s needed. Insulin secreted from the pancreas aids the transfer of sugar from blood into organs needing it for energy.
Type 1 diabetes is caused by failure of the pancreas to secrete insulin such that organs don’t get enough sugar to function. Consequently, fat and protein build up in the blood to supply energy for vital functions of the brain, muscles and other organs. Effects of excess fat and protein coupled with lack of sugar for brain, nerve and muscles eventually are fatal.
Type 2 diabetes is caused by lack of room to store sugar and fat in muscles and liver. Storing sugar and fat in fat tissue and extracellular spaces requires much more insulin than transfer into cells of muscle and liver. Consequently, more insulin is secreted by the pancreas but it’s often not enough to clear sugar and fat to safe levels in the blood.
 The usual cause for type 2 diabetes is adding more sugar and fat into the blood, day after day, until levels rise above what can be cleared into muscles and liver. The excess is transferred into fat tissue and into the extracellular spaces of muscles, liver and pancreas.
The usual cause for type 2 diabetes is adding more sugar and fat into the blood, day after day, until levels rise above what can be cleared into muscles and liver. The excess is transferred into fat tissue and into the extracellular spaces of muscles, liver and pancreas.
A normal healthy person transfers sugar, protein and fat from a meal that is not needed immediately into muscles and liver.
Insulin resistance. When the cells of muscles and liver are filled and there’s no more room, the extra nutrient is stored somewhere else. Clearance is slower and requires more insulin. That’s called insulin resistance.
Reduction of insulin secretion. Buildup of sugar and fat that doesn’t clear completely between meals and overnight causes the pancreas to secrete more insulin. When more insulin is increased in the blood, sugar and fat gets stored as fat in muscles, liver and pancreas. Extra fat stored in the pancreas blocks it from secreting enough insulin. Reduction of insulin secretion causes even less sugar and fat to be cleared from the blood.
 Increased insulin sensitivity. Physical work by muscle increases its needs for energy such that it increases the amounts of sugar and fat that it clears. Increased requirements for energy, day after day, increases the amounts of sugar and fat it clears even when it’s resting. That’s called increased insulin sensitivity.
Increased insulin sensitivity. Physical work by muscle increases its needs for energy such that it increases the amounts of sugar and fat that it clears. Increased requirements for energy, day after day, increases the amounts of sugar and fat it clears even when it’s resting. That’s called increased insulin sensitivity.
Aerobic exercise training. Muscle that works using energy beyond the sugar and fat it has stored, increases its clearance of fat and sugar from the blood while it’s working. Blood vessels dilate and circulation of blood increases the amounts of sugar and fat delivered. It also increases the amount of oxygen delivered while working. Work can be performed for minutes or even hours without stopping. This type of work is called aerobic exercise training.
Resistance exercise training. Muscle that is forced to work beyond amounts of energy immediately available stimulates its fibers to increase in strength. The duration it can continue working is limited by the amounts of energy it has stored. Between bouts of work, it stimulates its fibers to increase in bulk and store more energy. This type of work is called resistance exercise training.
Reversal of type 2 diabetes. Exercise that increases the amounts of energy muscle requires for its work increases daily requirements for calories in food and drink. When total requirements for energy exceed energy in the total calories consumed, stores of excess fat in muscle, liver and pancreas are depleted. When excess fat is depleted from these organs, levels of sugar and fat in the blood return to normal healthy levels between meals and overnight. That’s called reversal of type 2 diabetes.
Remission of Type 2 Diabetes
Remission means reducing concentrations of sugar and fat in the blood to normal healthy levels. These would be levels that are not associated with organ damage or disabling chronic diseases.
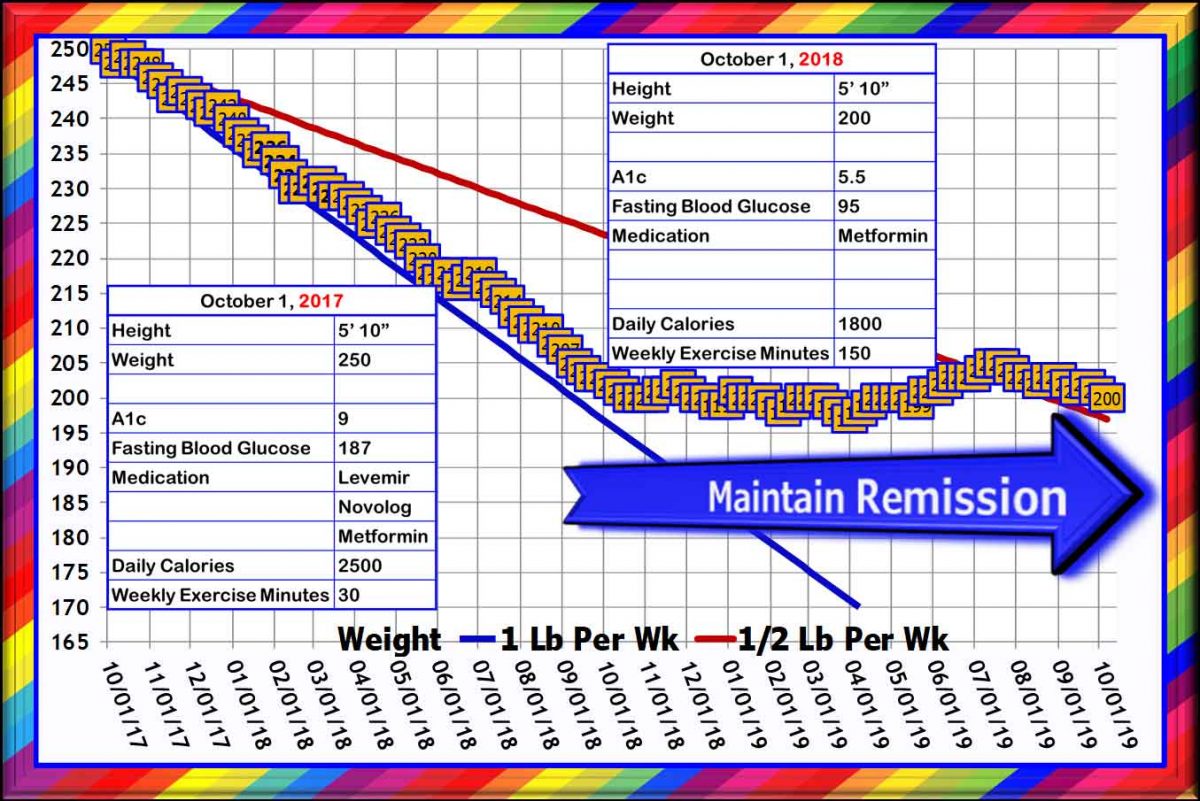
Investigators in the DiRECT diabetes remission trial defined remission as having an A1c <6.5% and discontinuing all diabetes medications for at least 2 months.
Investigators in the Look AHEAD intensive lifestyle intervention trial defined remission as having A1c <5.7%, fasting blood glucose <100 mg/dL and discontinuing all diabetes medications for at least 1 year.
Scientific opinion is that extra fat deposited in the liver due to weight gain, causes fat accumulation in the pancreas and impairs its production of insulin. The objective proposed is to reduce excess fat in the liver and pancreas.
DiRECT Diabetes Remission Trial
The DiRECT trial was done in primary care practices in the UK. Investigators recruited 298 individuals aged 20–65 years, with less than 6 years’ duration of type 2 diabetes, BMI 27–45, and not receiving insulin. Approximately 25% of the patients in private practices who qualified agreed to participate.
Subjects were divided into Control Group and Intervention Group with 149 subjects in each group.
The intervention consisted of withdrawal of antidiabetes and antihypertensive drugs, total diet replacement (825–853 kcal per day formula diet for 12–20 weeks), stepped food reintroduction (2–8 weeks), and then structured support for weight-loss maintenance.
 The first Figure shows that the average body weight for all subjects was about 200 lb. During the first 4 months, average body weight for subjects in the Intervention Group fell to about 175 lb. During the next 20 months, their average body weight increased to about 185 lb.
The first Figure shows that the average body weight for all subjects was about 200 lb. During the first 4 months, average body weight for subjects in the Intervention Group fell to about 175 lb. During the next 20 months, their average body weight increased to about 185 lb.
Subjects in the Control Group remained little changed at about 200 lb.
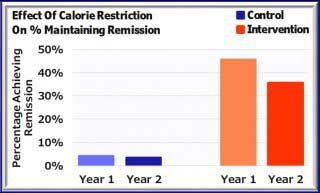
The first Figure below shows that during Year 1, 24% of the subjects in the Intervention Group reduced body weight more than 30 lb. During Year 2, 9% of those subjects had reduced weight more than 30 lb.
The second Figure below shows that during Year 1, 45% of those subjects had achieved remission. Those subjects had been in remission for at least 2 months. During Year 2, 35% were in Remission. Most of those 53 subjects had been in remission for at least 1 year.
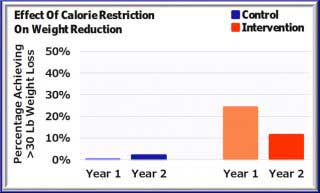
The next Figure shows that the % Achieving Remission was strictly proportional to the Amount of Weight Reduction. Approximately 70% of those who lost more than 30 lb achieved Remission that held for about 2 Years.
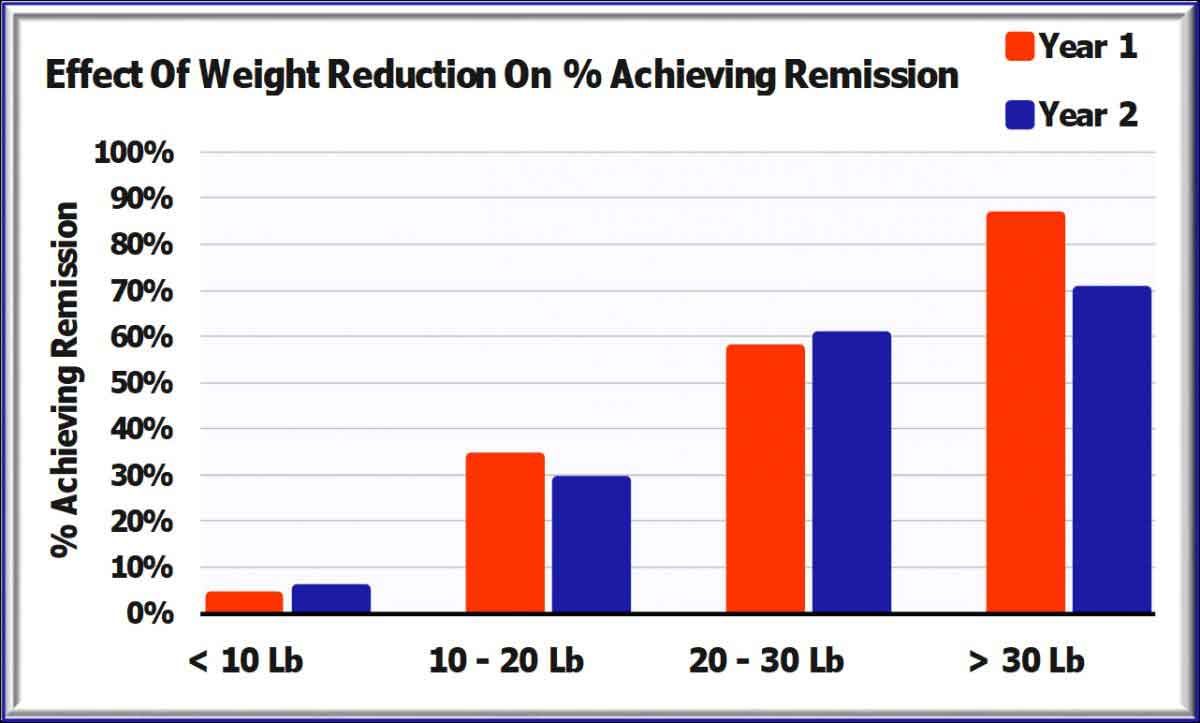
In the whole Study Population, including those in the Control Group, 64% of those subjects who maintained at least 20 lb weight loss achieved Remission.
More than 35% of subjects in the DiRECT Trial achieved Remission. However, 75% of the total eligible population rejected the opportunity to participate. The % of eligible patients in private practice who participated and achieved Remission was less than 5%.
Look AHEAD Intensive Lifestyle Intervention
The Look Ahead clinical study was done in 16 centers throughout the U.S. Investigators recruited 5,145 men and women aged 46–76 years with type 2 diabetes and BMI >25. Approximately 20% were taking insulin at baseline.
The objectives of the intervention were to achieve a mean loss >7% of initial weight and to increase physical activity to >175 minutes a week.
Half of the subjects were randomly assigned to Intensive Lifestyle Intervention with group and individual counseling every week in the first year and twice each month during 2nd to 4th years. Intensive Intervention consisted of instruction in nutrition and physical activity and social support.
Subjects in the Control Group were offered 3 group sessions each year.
The Figure shows total body weights of subjects in the Intensive Intervention Group at the end of Year 1 and after the end of Year 8.
At the end of Year 1, 93% had reduced weight at least -5%, 68% had reduced weight at least -5%, 38% had reduced weight at least -10% and 16% had reduced weight at least -15%.
By the end of Year 8, 74% had reduced weight at least -5%, 50% had reduced weight at least -5%, 27% had reduced weight at least -10% and 11% had reduced weight at least -15%.
As shown in the Figure, the subjects with the greatest success in retaining 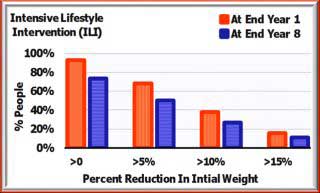 reduction in weight were those who reduced the most. Almost all of those who lost less than -5% weight during the first year, regained most of what they had lost. Those who lost at least -15% weight during the first year were all successful in retaining weight reductions of at least -10%.
reduction in weight were those who reduced the most. Almost all of those who lost less than -5% weight during the first year, regained most of what they had lost. Those who lost at least -15% weight during the first year were all successful in retaining weight reductions of at least -10%.
Remission of diabetes during Year 1 was achieved by 11.5% of subjects in the Intensive Intervention Group and by 7.3% at the end of Year 4. Continuous, sustained remission for 4 years was achieved by 3.5%.
Average physical activity reported at baseline by all subjects expended approximately 860 kcal per week. That represented approximately 15 min per day of moderate intensity exercise.
Energy expended by subjects in the Intensive Intervention Group more than 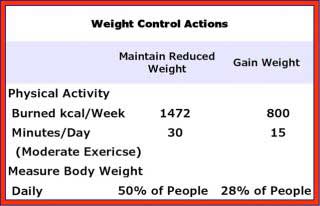 doubled in Year 1. Duration of moderate exercise was increased to about 40 minutes per day. However, intensity and duration decreased during the next 7 years. During Year 8, energy expended on physical activity was 1,472 kcal per week during exercise sessions lasting about 30 minutes per day.
doubled in Year 1. Duration of moderate exercise was increased to about 40 minutes per day. However, intensity and duration decreased during the next 7 years. During Year 8, energy expended on physical activity was 1,472 kcal per week during exercise sessions lasting about 30 minutes per day.
Subjects who did not lose weight or actually gained weight did not increase their physical activity during the study.
In addition, subjects who were successful in reducing weight measured their weight more often than subjects who did not lose weight. Approximately half of the subjects who lost weight measured their weight daily. Only approximately one quarter of the subjects who did not lose weight measured weight daily.
Exercise Training And Reduction Of Fat In Liver And Pancreas
Hepatic fat content is reduced by aerobic and resistance exercise training. Results of several clinical trials have demonstrated that exercise reduces fat content of the liver. In skeletal muscle, exercise reduces insulin resistance and decreases the excess sugar and fat delivered to the liver. In the liver, exercise increases metabolism and removal of fat from blood and liver.
Exercise is proven to be good treatment to improve fatty liver disease.
Pancreatic fat content and glucose tolerance respond to exercise training. Fat content of the pancreas can be measured by magnetic resonance spectroscopy.
Studies of men and women in Finland have demonstrated reductions in pancreatic fat content of normal, healthy men and fat content in the pancreas of men and women with type 2 diabetes.
Two weeks of exercise training decreased fat content in all subjects and improved both insulin-stimulated glucose and fatty acid uptake.
On Physical Examination, Maximum Waist Circumference is the most sensitive indicator of excess fat in liver and pancreas. It also is the most sensitive indicator of insulin sensitivity.
Effects of exercise on fat in liver and pancreas can be assessed by sequential measurements of maximum waist circumference.
Summary
The combination of Calorie Restriction and Exercise Training reverses diabetes all the way to complete remission.
Scientific opinion is that extra fat deposited in the liver is due to weight gain.
That weight gain causes fat accumulation in the pancreas and impairs its production of insulin.
The most success is achieved by substantial restriction of calories and vigorous daily exercise that get started right away.
Both strenuous exercise training and substantial calorie restriction remove fat from muscle, liver and pancreas. Improved insulin secretion and decreased insulin resistance maintain remission and prevent return of glucose intolerance.
Age by itself does not decrease energy requirements. As long as intensity and duration of daily exercise continue, requirements for daily calorie intake stay the same.
Maintaining remission of type 2 diabetes requires good health practice that continues indefinitely. That includes restraining calorie intake and enhancing energy output.
What’s essential is:
•Moderate intensity and duration of daily exercise,
•Adequate intake of protein, fiber and healthy fat,
•Avoidance of sugar, excess sodium and unhealthy fat.
Life is more enjoyable limiting excess calories and keeping active than having to consume less and exercise more.
 We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com