Telehealth Reverse Diabetes: Results of Bariatric Surgery | Free Trial In Texas
Body weight reduction for overweight/obese individuals improves health, reduces severity of type 2 diabetes and prolongs life.
Bariatric surgery, when successful in reducing body weight, greatly improves health, reduces severity of type 2 diabetes and substantially prolongs life.
Drug therapy and injection of insulin are essential to prevent diabetic ketoacidosis but they have little effect on reducing severity of cardiovascular disease in type 2 diabetes or prolonging life.
Metformin and lifestyle intervention prevents or delays onset of type 2 diabetes.
Improve your health practices, prevent or reverse type 2 diabetes and prolong life.
Sign UpTo learn more about programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
Cardiovascular Disease In Type 2 Diabetes
Managing levels of fat and sugar in the blood is important in patients with Type 2 Diabetes. If insulin secreted naturally by the pancreas is not effective in clearing fat and sugar from the blood, high levels of ketones build up. Ketones are toxic and cause confusion, coma and death. To prevent ketoacidosis from happening, levels of fat and sugar must be controlled even if that requires injecting insulin every day.
Complications of cardiovascular disease, when ketoacidosis is prevented, are the principal causes of death in patients with type 2 diabetes. Adults with diabetes have more than twice the risk of death from cardiovascular disease compared to those without diabetes. Because diabetes causes high levels of sugar and fat in the blood, it has always been assumed those high levels increase the risk of cardiovascular disease.
The objective of treating diabetes with insulin or other medications is lowering sugar levels in the blood. The aim is a pre-meal blood sugar of 90-130 mg/dl and blood sugar after meals of less than 180 mg/dl.
Effect of managing blood sugar with medications on cardiovascular disease has been disappointing. Effect of medication treatment on HbA1c in controlled clinical trials has been about -1% in 3 to 12 months. In spite of lowering blood sugar levels, insulin and other drugs for treatment of diabetes have shown little benefit in reducing cardiovascular disease and premature death.
 Most of the clinical trials using medications in the last 10 years have tested effects of newer agents on patients who already have complications of cardiovascular disease. These are patients who have been hospitalized for treatment of serious events. Some of these newer agents have been successful in reducing recurrences of heart attacks and strokes in those patients.
Most of the clinical trials using medications in the last 10 years have tested effects of newer agents on patients who already have complications of cardiovascular disease. These are patients who have been hospitalized for treatment of serious events. Some of these newer agents have been successful in reducing recurrences of heart attacks and strokes in those patients.
So far, there is no evidence that medication for reducing levels of blood sugar have any effect on initial development of cardiovascular disease. However, some of the newer agents have been successful in reducing body weight about 10% in 12 months. If this reduction in body weight can be maintained, there eventually may be some success in preventing cardiovascular disease and premature death.
Bariatric Surgery In Patients With Type 2 Diabetes
Surgery for reducing weight began in the 1950’s. The first operations bypassed most of the small intestines without affecting the stomach. Although successful in reducing weight, there were many complications. Since then, surgery has involved reducing the size of the stomach and bypassing the first part of the small intestine.
After surgery, most patients have a reduction in hunger and feel full after eating. However, rapid entry of food into the small intestine can cause gastrointestinal and metabolic symptoms. As a result, ultimate success depends on careful attention to principles of healthy eating.
Several small clinical trials have shown success in weight reduction, control of type 2 diabetes and reduced mortality. However, these were small trials of short duration. Not enough size and duration to assess morbidity and mortality from cardiovascular disease.
Recently, a clinical trial was conducted in adult patients with obesity and type 2 diabetes who had bariatric surgery within the Cleveland Clinic Health System. All these patients had surgery and follow-up from 1998 to 2018.
A total of 2,287 patients who had bariatric surgery were matched against 11,435 nonsurgical control patients. The average observation time was 4 years.
Improvement in Body Weight and HbA1c occurred within the first 2 years following bariatric surgery. Even after 8 years, the reduction in Body Weight was more than improvement seen in patients receiving nonsurgical treatment.
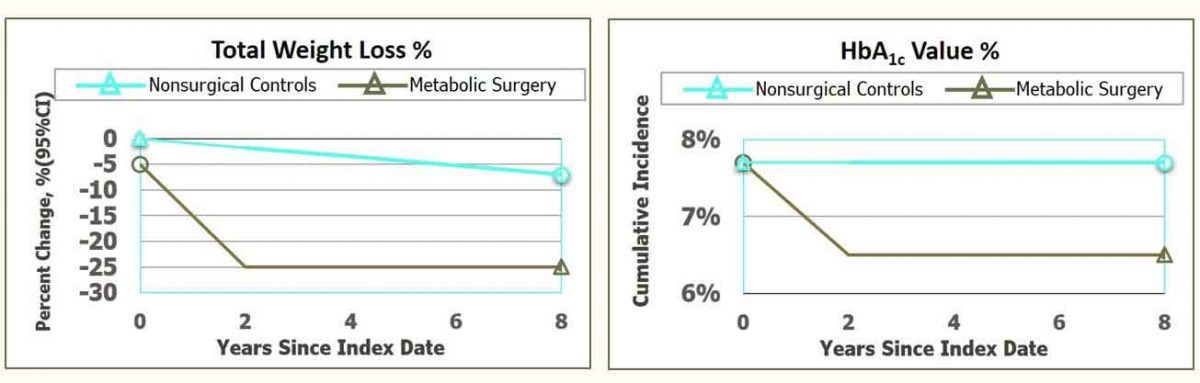
Note that reduction in Body Weight of -25% still left most patients in the Overweight category. Simply being Overweight doubled the risk of cardiovascular disease in patients with type 2 diabetes.
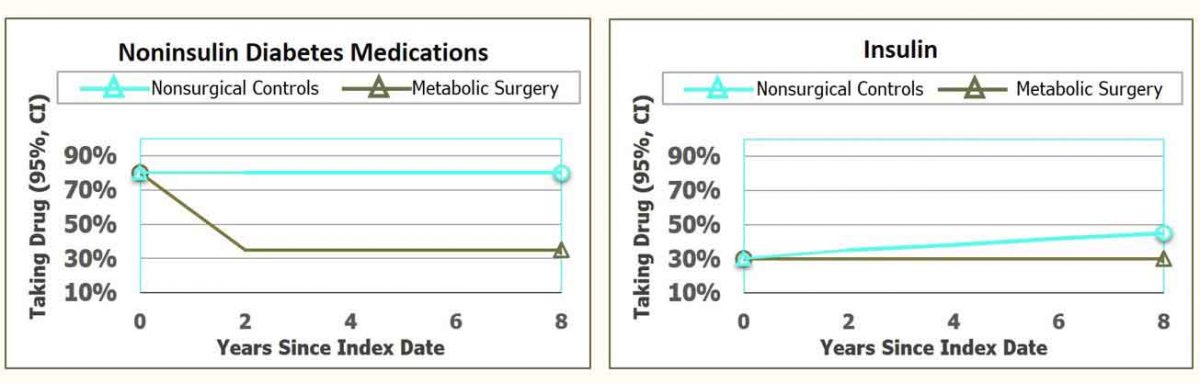
Reduction in HbA1c indicated that controlling levels of sugar in the blood was improved following bariatric surgery. Most patients receiving insulin and other drugs to reduce HbA1c required less medication. After bariatric surgery, most patients continued to receive insulin and other drugs but HbA1c was better controlled.
The Primary End Point was first occurrence of coronary artery events, cerebrovascular events, heart failure, atrial fibrillation, nephropathy, and all-cause mortality.
The Secondary End Point included all-cause mortality, myocardial infarction, and ischemic stroke.
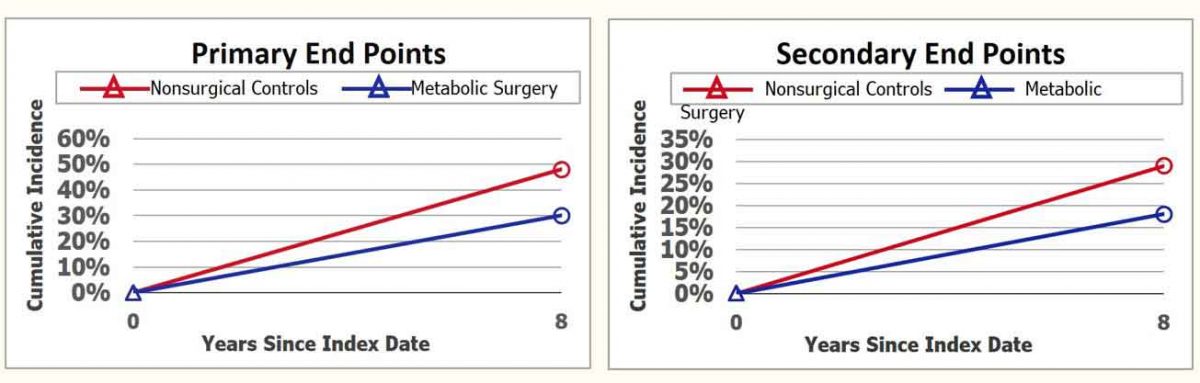
Note that the rate for Primary End Points for patients after bariatric surgery was 40% lower than obese patients without surgery. However, the rate of almost 20% major events after 8 years is still terribly high. More than twice the rate that would be expected for adults of average healthy weight who do not have diabetes.
All-cause Mortality rates, of course, include more causes of death than deaths from cardiovascular disease by itself. The final rate is still alarmingly high. Again indicating the dangers of overweight and obesity.
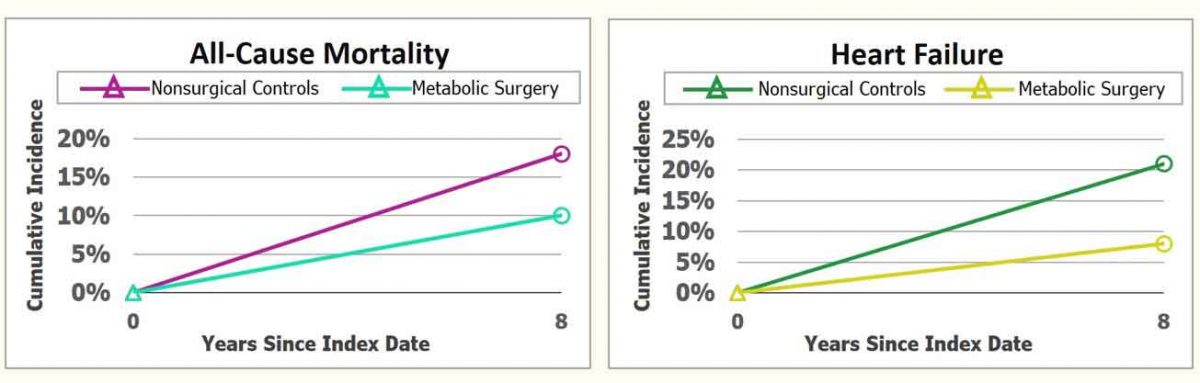
The improvement in development of heart failure after bariatric surgery indicates the high risk of heart failure caused by obesity.
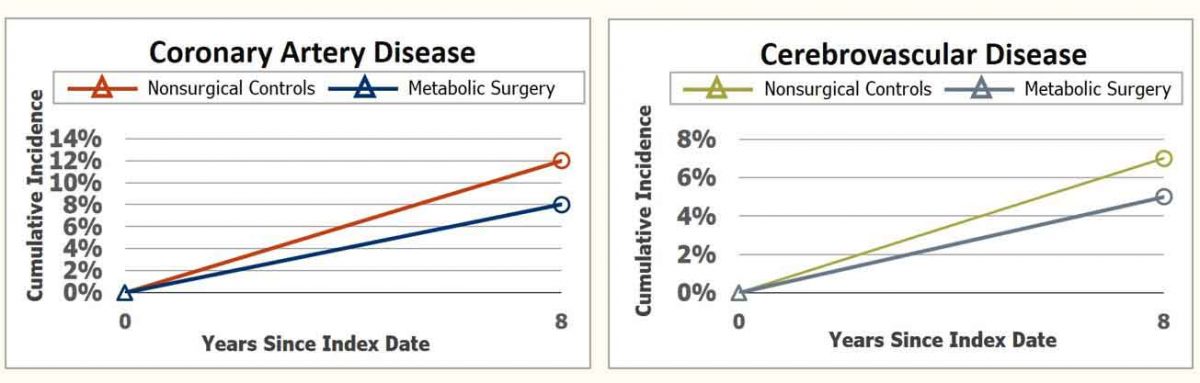
Rates of coronary artery disease and cerebrovascular disease following bariatric surgery were both improved by about 30%. Of course, the development of either form of vascular disease greatly shortens predicted length of life. The best that can be said is that they escaped death during the follow-up study.
Development of Chronic Kidney Disease and Atrial Fibrillation (Abnormal Heart Rhythm) were significantly decreased following bariatric surgery. Especially development of Chronic Kidney Disease which was decreased to 6%.
Chronic Kidney Disease as a cause of death in patients with diabetes is second only to cardiovascular disease. Approximately one third of all patients with type 2 diabetes and obesity develop Chronic Renal Disease. Bariatric surgery greatly decreased that risk.
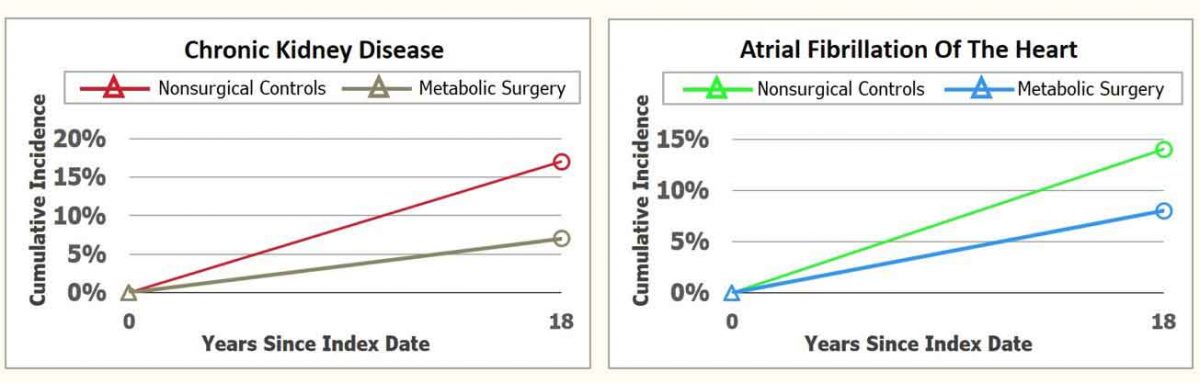
Atrial Fibrillation more than doubles the risk of heart failure and the risk of stroke. Decreasing the development of Atrial Fibrillation after bariatric surgery greatly decreased the risk of death from heart failure and stroke.
Medication to Control Blood Pressure and Lipid Metabolism was decreased almost 50% following bariatric surgery. This shows the effect of obesity on the kidneys and constriction of arterial vessels causing hypertension and renal failure.
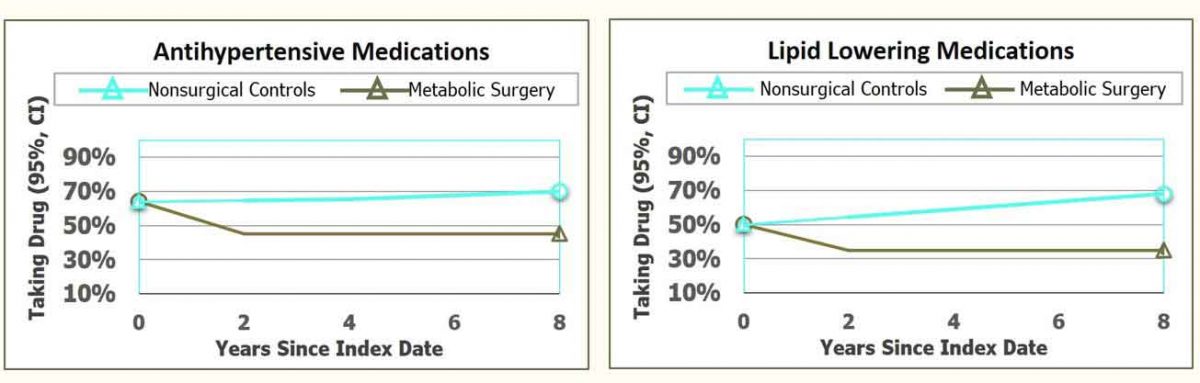
The improvement in Lipid Metabolism shows the marked effect of obesity and diabetes to increase levels of fat circulating in blood.
Complications after Bariatric Surgery
Following surgery, the transition to regular food requires about 10 weeks. Progression begins from liquids for 3 weeks to pureed and soft foods until soft solid foods can be tolerated. From then on, only small portions of food can be eaten and solids and liquids consumed separately.
Complications include gastric ulcer, gallstone formation and gastrointestinal disturbances. The rapid entry of food into the small intestine that distends the gut causes symptoms and release of excess insulin causing low blood sugar.
To avoid regaining weight, only small amounts of food can be eaten.
Remission of Type 2 Diabetes
As shown in the Figures for HbA1c and requirements for medication, bariatric surgery does not reverse obesity and type 2 diabetes enough for remission in most patients. Those who get the best results are those with the most severe obesity at the time when type 2 diabetes appeared along with substantial reductions in % Body Fat. As a result, the predictors for remission include healthy eating and vigorous physical activity.
Criteria for success represent preserved pancreatic beta-cell function, and potential for reduction in insulin resistance.
Indicators for preserved pancreatic beta-cell function, include:
• younger age,
• shorter duration of diabetes, and
• higher C-peptide level (a laboratory test indicating production of insulin).
The potential for reducing insulin resistance includes:
• higher baseline BMI,
• high proportion of body fat, and
• large amount of abdominal visceral fat.
Summary
Bariatric surgery along with remarkable and sustained weight reduction is a reasonable option for reversing diabetes in young, morbidly obese patients.
Remission will persist as long as normal body weight is sustained.
The best possible treatment for type 2 diabetes is healthy weight and body composition, healthy routine of moderate exercise, healthy sleeping and pleasurable interpersonal and social relations.
Let us help you achieve that best possible treatment.
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com