Telehealth Reverse Diabetes To Complete Recovery | Free Trial In Texas

Type 2 diabetes is a situation, not a disease. It’s taking in more energy than can be used or quickly stored. Some people run out of storage space for excess energy more quickly than others.
Being too short to make the basketball team is a situation. It’s not a disease. Wearing high heels doesn’t help playing basketball.
Insulin doesn’t fix anything. It just forces excess energy into new storage space more quickly.
Complete recovery from type 2 diabetes is balancing energy intake, output and storage permanently without medication.
Sign UpTo learn more about programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
Defining Type 2 Diabetes
The World Health Organization describes diabetes as a chronic disease that occurs when the pancreas does not produce enough insulin or alternatively, when the body cannot effectively use the insulin it produces.
About 90% of people with diabetes around the world have type 2. It is recognized to be largely the result of excess body weight and physical inactivity.
It is not a disease. It is not ineffective use of insulin. It is the result of more energy than the body can use or store.
What causes excess body weight? Overeating. More energy consumed than can be used or quickly stored. Normal sites of quick storage are in skeletal muscle and liver. Slower storage occurs in subcutaneous fat tissue.
There is a normal range of storage capacity for excess energy. Just as there is a normal range of height for adult men and women. Type 2 diabetes very seldom occurs with low normal % body fat (<20% for males and <30% for females) along with high normal % skeletal muscle (>40% for males and >30% for females).
What has to be managed is energy intake in relation to energy output and sites of temporary energy storage.
Recovery From Type 2 Diabetes
Distinctions between reversal, successful treatment, remission, recovery and cure are confusing.

If type 2 diabetes is defined as high levels of blood sugar, lowering them could be called “reversal.” Normalizing those levels by lifestyle and medication could be “successful treatment.” If non-diabetes levels are attained and maintained without anti-diabetes drugs, that could be “remission.” If normal levels of blood sugar and a healthy balance between energy input, output and storage is regained without medication, then “recovery” seems more accurate.
If there never was anything wrong except overeating along with physical inactivity, then what was ever there to be cured? Possibly transplant of pancreas tissue replacing absent or defunct insulin-secreting cells could be called “cure.”
A consensus group of experts in diabetes met in 2009 to figure this all out. After much discussion, remission was defined as disappearance of the signs and symptoms of disease with no active anti-diabetes drug therapy or ongoing procedures for at least 1 year.
Disappearance of abnormal blood sugar values was defined as Fasting Blood Sugar < 100 mg/dL and HbA1c <5.7%.
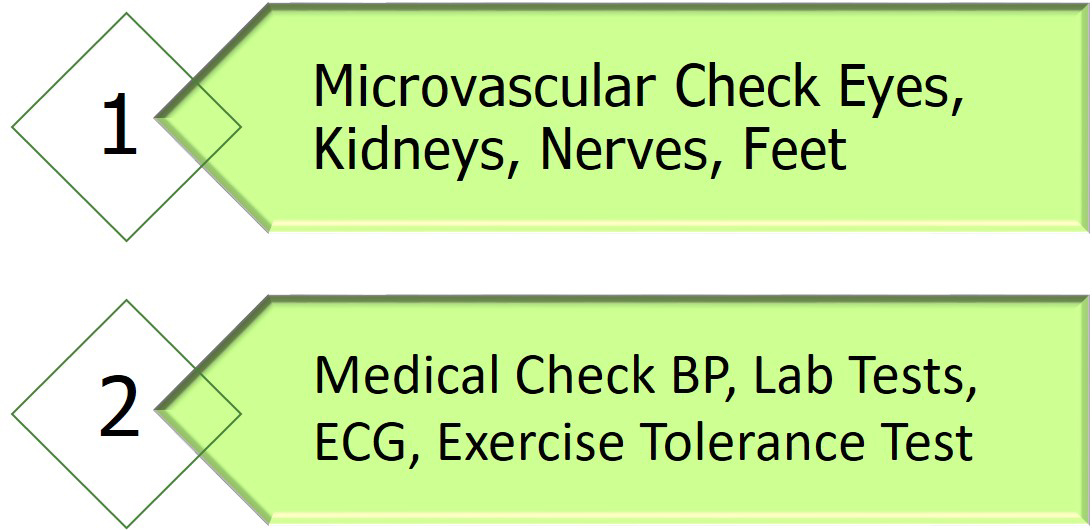
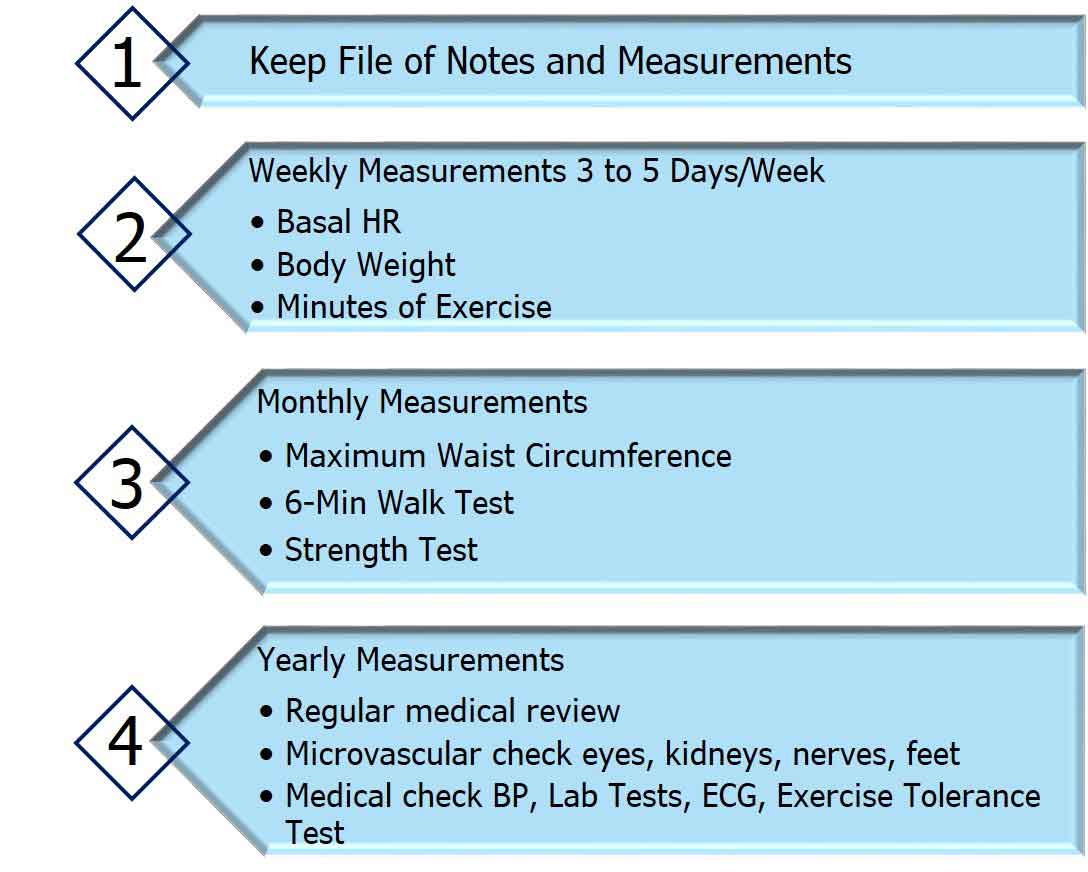
Implicit in the statement is the possibility for recurrence of the disease. Therefore, the Expert Group recommended remission of less than 5 years’ duration be monitored by continued regular screening for microvascular complications. After 5 years with no history of a complication, screening could be reduced to schedules for individuals with no history of diabetes.
Position statement of experts in the UK meeting in March, 2019. This meeting was organized by the Association of British Clinical Diabetologists (ABCD) and the Primary Care Diabetes Society (PCDS). They proposed fasting blood sugar levels below the threshold currently used for diagnosis of type 2 diabetes (126 mg/dL) for at least 6 months without any anti-diabetes drug treatment.
Because the effects of an elevated A1C (>6.2%) can be damaging to microvascular function, the experts recommended continued screening for nerve, kidney, and eye damage for at least five years. Also recommended were frequent screenings for cardiovascular disease.
The Personal Fat Threshold with type 2 diabetes is similar in obese and non-obese individuals. Studies of insulin resistance in groups with type 2 diabetes or normal glucose tolerance show similar results for obese and non-obese subjects. The relative difference in insulin resistance is similar. Also, non-obese people reverse their diabetes after weight loss in the same proportions as obese people.
Reversal of type 2 diabetes apparently is associated with a reduction in pancreatic fat levels. Insulin resistance simply develops in relation to individual thresholds of tolerance for excess calorie intake. About 50% of individuals with type 2 diabetes tolerate greater accumulation of % body fat than non-obese individuals.
Recovery From Insulin Resistance
Change in body weight affects insulin resistance. Data from routine health checks show increased insulin resistance with increase in weight. As little as 4 or 5 pounds increase in 1 or 2 years increases insulin resistance enough to increase fasting blood sugar levels above 100 mg/dL. Decrease in weight reduces insulin resistance.
Body weight has little effect on responses to change. Increase and decrease in insulin resistance and fasting blood sugar values occurs with body weight in the normal healthy range as well as with overweight and obesity.
Weight reduction with exercise and calorie restriction improves insulin sensitivity. Studies in overweight men and women show favorable effects of each separately. Combined exercise and calorie restriction produce twice the increase insulin sensitivity with the same reductions in weight of either alone.
Benefits of reducing insulin resistance combined with improved secretion of insulin make calorie restriction and physical activity powerful mediators of recovery from type 2 diabetes.
Resting Heart Rate and Insulin Resistance
Insulin resistance correlates strongly with resting heart rate. Because heart rate is controlled by the autonomic nervous system it’s possible that the brain is stimulating insulin secretion. It’s also possible that insulin is stimulating the nervous system.
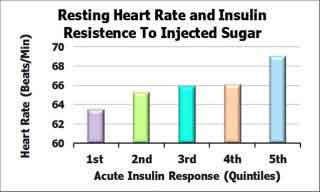 The relation between resting heart rate and insulin resistance has been studied in 137 young men and women in the UK. Resting heart rate was measured after 30 minutes lying down in a quiet room. Insulin resistance was measured using measurements of insulin in blood samples following intravenous injection of sugar (225 mg of glucose per pound of body weight).
The relation between resting heart rate and insulin resistance has been studied in 137 young men and women in the UK. Resting heart rate was measured after 30 minutes lying down in a quiet room. Insulin resistance was measured using measurements of insulin in blood samples following intravenous injection of sugar (225 mg of glucose per pound of body weight).
The level of insulin in blood following injection of sugar indicates the resistance of skeletal muscle and liver to quickly clear the blood of sugar. As shown in the Figure, those individuals with the lowest resting heart rates had the least insulin response following injection of sugar.
High overnight heart rate measured by other investigators has shown a strong association with the insulin resistance syndrome.
Successful Maintenance Of Recovery
The Look AHEAD study randomly assigned 5,143 overweight/obese subjects to education and intensive coaching to promote weight loss through decreased calorie intake and increased physical activity. Intensive intervention resulted in an 8.6% weight loss the first year and nearly 5% at 4 years. Those subjects who reduced weight more than 10% the first year were the most successful in maintaining weight loss during 4 years of follow-up.
The National Weight Control Registry is an ongoing, observational study of individuals who have achieved long-term success in weight loss maintenance. Individuals are eligible to join the program if they have maintained a weight loss of at least 30 pounds for at least 1 year.
The general conclusion from the study so far is that restricting calorie intake and increasing exercise are essential to success. No particular diet or exercise routine stands out as particularly effective over all other programs.
The majority of successful individuals follow 3 health practices.
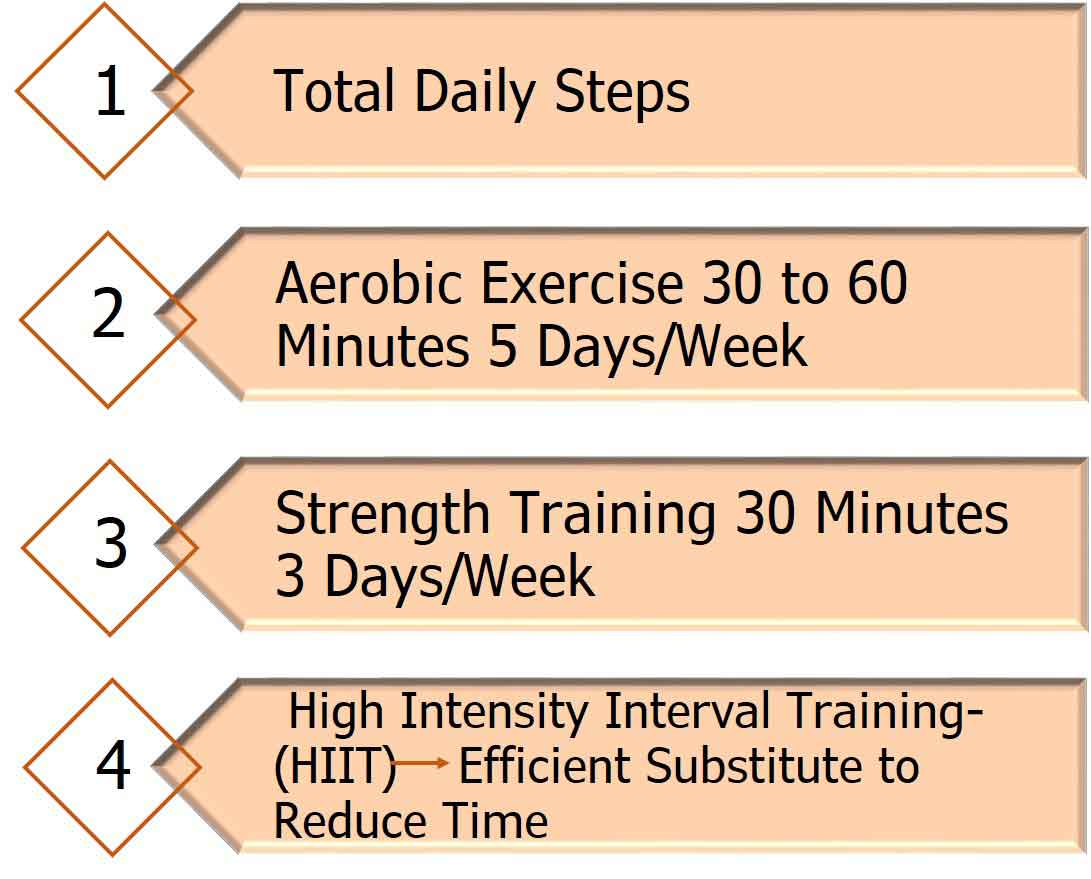
High levels of physical activity. The average amount of time spent in moderate and strenuous exercise is approximately 60 minutes per day. Substantially more than the 150 minutes per week recommended by health and fitness experts.
Food intake low in total calories. Most report meals and snacks low in fat and high in carbohydrates.
Regular self-monitoring of weight.
Those who maintain a weight loss for 2 to 5 years have the best chances of long-term success.
Strategy For Long-term Recovery From Type 2 Diabetes
Establish the best possible baseline recovery state.
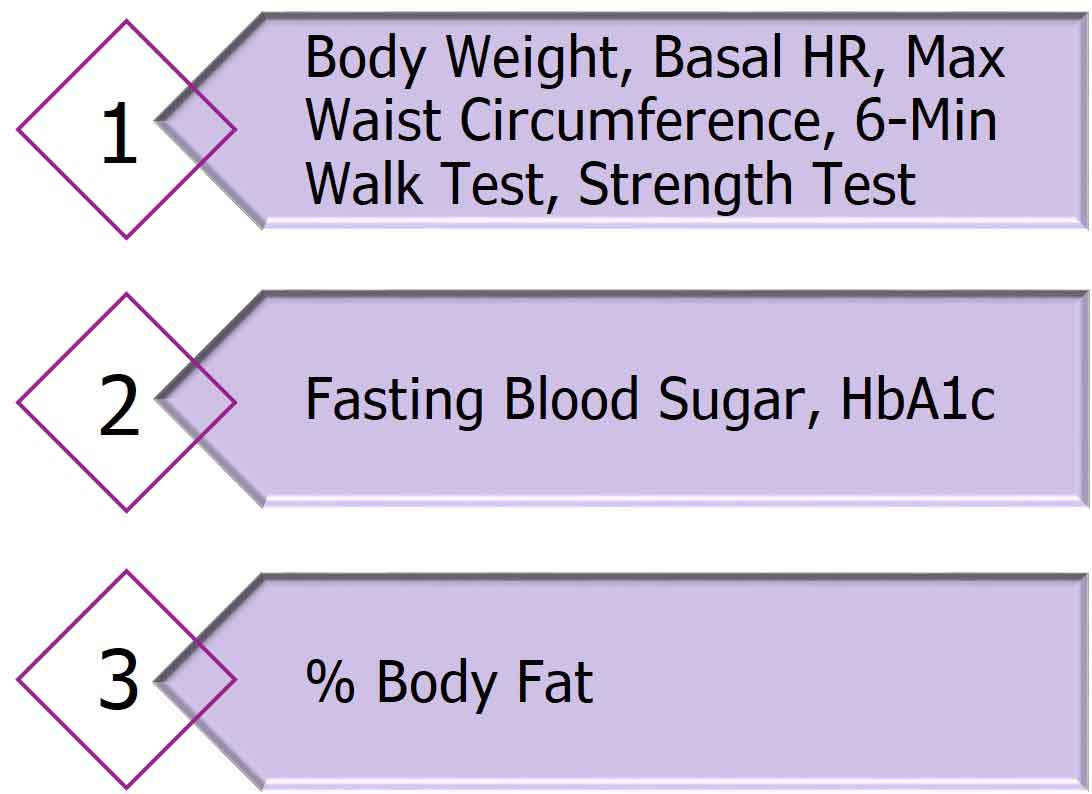
Schedule regular medical review.
Meal plan you can follow forever.

Exercise Routine you can follow forever.
Sleep 7 to 9 hours every night.
Don’t Smoke Tobacco.
Self-monitor.
Summary
Type 2 diabetes is the result of overeating. More energy consumed than can be used or quickly stored. Normal sites of quick storage are in skeletal muscle and liver. Slower storage occurs in subcutaneous fat tissue.
There is a normal range of storage capacity for excess energy. Just as there is a normal range of height for adult men and women.
What has to be managed is energy intake in relation to energy output and sites of temporary energy storage.
Remission of type 2 diabetes has been defined as disappearance of the signs and symptoms of disease with no active anti-diabetes drug therapy or ongoing procedures for at least 1 year.
Normal blood sugar values have been defined as Fasting Blood Sugar < 100 mg/dL and HbA1c <5.7%.
Weight reduction with exercise and calorie restriction improves insulin sensitivity.
Insulin resistance correlates strongly with resting heart rate.
Success in recovery follows 3 health practices.
•High levels of physical activity.
•Food intake low in total calories.
•Regular self-monitoring of weight.
Let us help you recover good health and maintain recovery with good health practices.
 We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com